Translate this page into:
Pharmacist assessment of patient safety culture in a Nigeria’s healthcare hub
*Corresponding author: Godwin Odey Olim, Department of Pharmacy, Obafemi Awolowo University Teaching Hospital Complex, Ile-Ife, Nigeria. olimgody@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Olim GO, Eniojukan JF, Saliu S, et al. Pharmacist assessment of patient safety culture in a Nigeria’s healthcare hub. Am J Pharmacother Pharm Sci 2025:005.
Abstract
Objectives
The main objective of this study was to determine the perspective of the pharmacy staff on patient safety culture and to identify areas of strength and weakness in safety culture.
Materials and Methods
The study was a cross-sectional survey conducted among pharmacy staff who were directly involved with the provision of pharmaceutical services to patients in a tertiary healthcare facility in South-West, Nigeria. Data were collected using the Agency for Healthcare Research and Quality Questionnaire. A purposive sampling technique was used to randomly administer the questionnaire to 82 pharmacy personnel who had direct professional interactions with patients. Analysis of data was done using the Statistical Package for the Social Sciences version 25.
Results
More than 80% of respondents were professionals (pharmacists/Internees) who were directly involved in providing pharmaceutical services in the department; 50% of respondents had worked in the pharmacy department from 1 year to <12 years and 56.1% worked more than 40 h per week. Overall, positive responses were satisfactory for teamwork (66.7%), overall perception of patient safety (61.0%), patient counseling (81%), and organizational learning (56.1%) but poor for staffing, work pressure and pace (26.8%), and communication about prescription across shifts (40.7%). Patient safety in this pharmacy received an overall rating of 62.2%.
Conclusion
There is a need for urgent attention of the management of the hospital to be drawn toward the need for re-evaluation of current safety culture composites and amend systems where necessary to reduce risks and improve pharmacy patient safety.
Keywords
Hospital
Nigeria
Pharmacy
Patient
Safety
INTRODUCTION
A crucial element and foundational element in assessing the quality of healthcare is patient safety. “The absence of avoidable harm to a patient during the provision of healthcare and reduction of risk of preventable harm associated with care to an adequate minimum” is how the World Health Organization defines patient safety.[1] The growing interest in this area has prompted studies aimed at evaluating and recording organizational traits that may have an influence on patient safety.[2] In a tertiary healthcare center, the pharmacy plays a critical role in ensuring patient safety. In an effort to avoid medication mistakes, it guarantees that patients take their drugs safely. Medication mistakes endanger patient safety and are a serious public health concern.[3] Every year, adverse drug events (ADEs) cause injuries or deaths in over 770,000 patients; more than 25% of these occurrences are the result of avoidable prescription mistakes.[4] Pharmacist intervention is thought to be able to prevent nearly half of these ADEs.[5] Hence, it is evident that pharmacists play a pivotal role in mitigating medication errors and subsequently enhancing patient outcomes.[6]
By raising staff knowledge of patient safety concerns and highlighting areas for strength and progress, hospital pharmacists’ safety culture has the ability to greatly boost organizational quality improvement programs. This becomes more and more important when pharmacists take on responsibilities beyond just filling prescriptions.[7,8]
The Agency for Healthcare Research and Quality (AHRQ) pilot research outlined pharmacies’ advantages and disadvantages with regard to patient safety.[9] Furthermore, research from a number of nations has assessed the patient safety culture in community pharmacy settings using the AHRQ survey.[10-13]
As hospital pharmacists and their support personnel are the front-line providers of care, especially for in-patients, it is critical to guarantee patient safety when using medications. Examining their viewpoints about the patient safety culture in their practice environments becomes essential.
Therefore, the principal aim of this research was to determine the pharmacy staff ’s perspective on patient safety culture at the teaching hospital. The purpose of the study was to determine the hospital pharmacy’s patient safety culture’s strong points and areas in need of development.
MATERIALS AND METHODS
Study design and setting
This cross-sectional survey was conducted at the Obafemi Awolowo University Teaching Hospital Complex (OAUTHC), in Ile-Ife, Osun state, to find out how pharmacy staff members felt about patient safety. The Obafemi Awolowo University, located in Ile-Ife, is associated with the teaching hospital. The hospital serves the people of the state and its surroundings by offering a range of specialist healthcare services.
Study population and sample size
The pharmacy personnel at OAUTHC comprises about 60 pharmacists of various cadres, 25 intern pharmacists, 15 pharmacy technicians, and 20 other supporting staff. However, excluding the supporting staff (since they do not have direct interactions with patients), the total population was 100. To obtain a suitable sample size for the study, Yamane’s formula was adopted.[14]
A sample size of 80 was obtained. However, 5% overage was added to account for errors and questionnaires that may not be returned or not completely filled; hence 84.
Data collection and sampling technique
The AHRQ Pharmacy Safety Questionnaire was modified and used for this investigation. There were 36 items in the survey instrument, measuring across 11 composites. In addition to the composites, the pharmacy survey included four items that focused on the background characteristics of the respondents, three items that asked how frequently different sorts of errors were documented, and an overall rating question.
Eighty-four employees working in the pharmacy sector, which provides pharmaceutical services, were randomly given the survey instrument. Because the sampling was done with a purpose, only pharmacy technicians, pharmacists, and intern-pharmacists who had direct professional encounters with patients were chosen at random.
Data analysis
Filled questionnaires were retrieved and coded into a Microsoft Excel package. Data were sorted for completeness and exported for analysis into the Statistical Package for the Social Sciences (version 25). Data were analyzed for descriptive statistics; presented in frequency and percentage. Statistical evidence for the use of 84 pharmacy staff was obtained from the sample size calculation based on the population of pharmacy personnel in the hospital.
RESULTS
The study had a response rate of 97.6% (82/84).
Background profile of the respondents
Out of 82 respondents, 51 (62.2%) were male, and Pharmacists and Pharmacy Interns were 50 (61.0%) and 20 (24.4%), respectively [Table 1].
| Item | Frequency (n) | Percentage |
|---|---|---|
| Gender | ||
| Male | 51 | 62.2 |
| Female | 31 | 37.8 |
| Staff position | ||
| Pharmacists | 50 | 61.0 |
| Intern pharmacists | 20 | 24.4 |
| Pharmacy technicians | 12 | 14.6 |
| How long staff have worked | ||
| <6 months | 2 | 2.4 |
| 6 months–1 year | 31 | 37.8 |
| 1 year–3 years | 15 | 18.3 |
| 3 years–6 years | 12 | 14.6 |
| 6 years–12 years | 14 | 17.1 |
| More than 12 years | 8 | 8.9 |
| How many hours staff work per week | ||
| 1–16 h | Nil | Nil |
| 17–31 h | Nil | Nil |
| 32–40 h | 36 | 43.9 |
| More than 40 h | 46 | 56.1 |
Patient safety survey items and culture composites
Average positive responses were satisfactory for teamwork (66.7%), perception of patient safety (61.0%), patient counseling (81%), and organizational learning (56.1%) [Table 2].
| S/N | Composites/items | Negative response n (%) | Neutral response n (%) | Positive response n (%) | % Average positive response |
|---|---|---|---|---|---|
| 1 | Physical space and environment | ||||
| A1. This drugstore is orderly. | 41 (50.0) | 5 (6.1) | 36 (43.9) | 44.7 | |
| A5. There is no clutter in this drugstore. | 34 (41.5) | 13 (15.9) | 35 (42.7) | ||
| A7. The physical design facilitates efficient work flow | 28 (34.1) | 15 (18.3) | 39 (47.6) | ||
| 2 | Teamwork | ||||
| A2. Employees respect one another. | 11 (13.4) | 6 (7.3) | 65 (79.3) | 66.7 | |
| A4. Employees are aware of their duties explicitly. | 28 (34.1) | 8 (9.8) | 46 (56.1) | ||
| A9. Employees collaborate as a cohesive team | 17 (20.7) | 12 (14.6) | 53 (64.6) | ||
| 3 | Staff training and skills | ||||
| A3. Technicians undergo work-related training. | 28 (34.1) | 18 (22.0) | 36 (43.9) | 53.4 | |
| A6. Employees are capable of performing their duties properly. | 12 (14.6) | 16 (19.5) | 54 (64.8) | ||
| A8. Adequate orientation is given to new employees | 30 (36.6) | 9 (11.0) | 43 (52.4) | ||
| A10. This pharmacy provides enough training for its staff. | 23 (28.0) | 16 (19.5) | 43 (52.5) | ||
| 4 | Communication openness | ||||
| B1. Staff opinions and recommendations are respected | 30 (36.6) | 26 (31.7) | 26 (31.7) | 47.6 | |
| B5. Employees are at ease posing inquiries. | 4 (4.9) | 30 (36.6) | 48 (58.5) | ||
| B10. Staff members find it simple to raise concerns about patient safety with their supervisor. | 13 (15.9) | 26 (31.7) | 43 (52.5) | ||
| 5 | Patient counseling | ||||
| B2. We advise patients to consult with pharmacists. | 16 (19.5) | 19 (23.2) | 47 (57.3) | 52.0 | |
| B7. Our pharmacists converse with patients for an adequate amount of time B11. Our pharmacists provide patients with crucial information on their new prescriptions | 22 (26.8) | 25 (30.5) | 35 (42.7) | ||
| B2. We advise patients to consult with pharmacists. | 9 (11.0) | 27 (32.9) | 46 (56.1) | ||
| 6 | Staffing, work pressure, and pace | ||||
| B3. Employees take enough breaks during their work hours. | 40 (48.8) | 14 (17.1) | 28 (34.1) | 26.8 | |
| B9. When processing medications, we feel hurried. | 23 (28.0) | 15 (18.3) | 44 (53.7) | ||
| B12. Our workforce is sufficient to manage the task. | 54 (65.9) | 18 (22.0) | 10 (12.1) | ||
| B16. Staff members find it challenging to perform effectively at this pharmacy due to interruptions and distractions | 39 (47.6) | 37 (45.1) | 6 (7.3) | ||
| 7 | Communication about prescriptions across shifts | ||||
| B4. We have explicit guidelines for the sharing of crucial prescription data across shifts. | 20 (24.4) | 22 (26.8) | 40 (48.8) | 40.7 | |
| B6. We have established protocols for exchanging prescription data between shifts. | 26 (31.7) | 21 (25.6) | 35 (42.7) | ||
| B14. There is good communication about the status of problematic prescriptions between shifts. | 26 (31.7) | 31 (37.8) | 28 (30.5) | ||
| 8 | Communication about mistakes | ||||
| B8. Employees at this drugstore talk about errors | 30 (36.6) | 31 (37.8) | 21 (25.6) | 42.3 | |
| B13. Staff members talk about patient safety concerns when they arise in this pharmacy B15. Here at this drugstore, we discuss how to avoid making the same mistakes twice. | 23 (28.0) | 23 (28.0) | 36 (44.0) | ||
| B8. Employees at this drugstore talk about errors | 17 (20.7) | 18 (22.0) | 47 (57.3) | ||
| 9 | Response to mistakes | ||||
| C1. When employees make mistakes, they get fair treatment. | 16 (19.5) | 21 (25.6) | 45 (54.9) | 50.0 | |
| C4. Rather than penalizing employees, this pharmacy encourages them to grow from their errors C7. We examine employee behavior and operational procedures to determine the root causes of errors in our pharmacy. | 5 (6.1) | 30 (36.6) | 47 (57.3) | ||
| C8. Employees believe that their errors are being used against them (R) | 5 (6.1) | 24 (29.3) | 53 (64.6) | ||
| C1. When employees make mistakes, they get fair treatment. | 35 (42.7) | 28 (34.1) | 19 (23.2) | ||
| 10 | Organizational learning | ||||
| C2. When an error occurs, we attempt to determine which issues in the workflow caused the error. | 18 (22.0) | 13 (15.9) | 51 (62.1) | 56.1 | |
| C5. When the same error occurs again, we adjust our procedures. | 13 (15.9) | 20 (24.4) | 49 (59.8) | ||
| C10. This drugstore has changed for the better as a result of mistakes | 10 (12.2) | 34 (41.5) | 38 (46.3) | ||
| 11 | Overall perceptions of patient safety | ||||
| C3. This pharmacy prioritizes sales over patient security. | 54 (65.9) | 12 (14.6) | 16 (19.5) | 61.0 | |
| C6. This pharmacy does a fantastic job of avoiding errors. | 19 (23.2) | 14 (17.1) | 49 (54.8) | ||
| C9. A major emphasis on patient safety is evident in the way we conduct business in our pharmacy. | 18 (22.0) | 13 (15.9) | 51 (62.1) | ||
Documenting mistakes at the pharmacy
A total of 38 (46.3%) respondents had a negative opinion, 19 (23.2%) had a neutral opinion while 25 (30.5%) had a positive opinion about documenting when a “mistake reaches the patient and could cause harm but does not” [Figure 1].
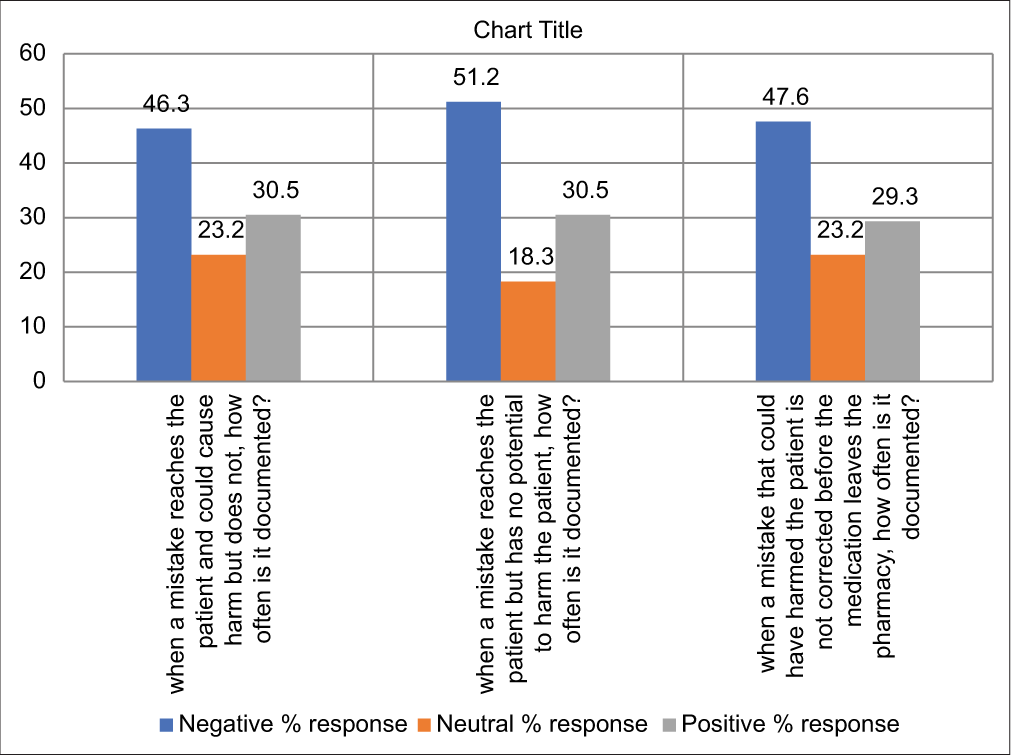
- Documentation of mistakes at the pharmacy
Assessment of the pharmacy’s overall rating on patient safety
Out of 82 respondents, 31 respondents rated the pharmacy poor/fair. A good rating was recorded from 25 respondents while 26 respondents rated the pharmacy very good/excellent. The percentage response of the rating is shown in Figure 2.
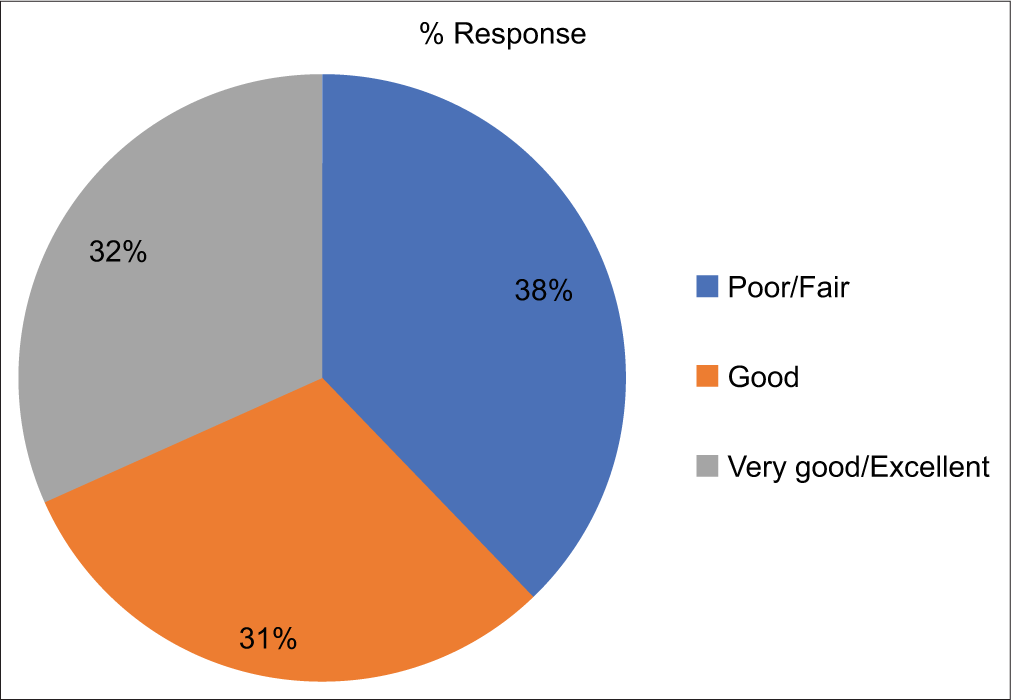
- Percentage overall rating of the respondents on patient safety
DISCUSSION
Evaluation of safety practices
Physical space and environment
Close to half of the respondents (44.7%) were optimistic about this safety culture composite. This is in contrast to a survey that recorded 70% positive opinion among respondents in a tertiary hospital in south-south, Nigeria.[14] It was observed that neither of the items in this composite had up to half a positive response by the respondents; indicating that the physical space and environment of the pharmacy need to be improved. A properly laid out pharmacy will remove clutters, improve good workflow, and enhance patient safety.
Teamwork and staff training and skills
In consonance with a previous study done in Nigeria, this safety culture composite recorded the best positive rating of 66.7%.[15] Patient safety, a multifaceted and intricate subject, demands a collaborative, multidisciplinary approach. The success of patient safety initiatives hinges on the collective efforts of a team. The research underscores that inadequate communication among team members forms the foundation of many medical errors.[16,17] Teamwork, conversely, has demonstrated associations with heightened patient safety, gaining increasing endorsement from healthcare policymakers as a means to ensure quality and safety in service delivery.[18,19] Effective teamwork contributes to improved decision-making, enhanced products, or services, and fosters a deeper sense of cohesion among team members over time. The satisfaction ratings of team members correlate with the level of teamwork processes present.[20] In terms of staff training and skills, the composite received an average rating of 53.4%. It is emphasized that all health professionals engaged in patient counseling should possess a solid foundation in basic and ongoing education.[21]
Communication openness
The positive rating for this composite was below average (47.3%). Although two out of three items recorded a positive response from up to half of the respondents, the average percentage was below 50%. Odd among the items was the positive response for “staff ideas and suggestions being valued in the pharmacy” (31.7%). This item was sore and not up to a third of the respondents submitted a positive response. In an organizational culture of this nature, staff members frequently hesitate to report adverse events and unsafe conditions due to concerns about potential reprisals or a belief that reporting won’t lead to any meaningful change.[22]
Patient counseling
In general, the patient counseling culture in this pharmacy was good with an average positive composite score of 52.0%. What draws much attention is the positive response for pharmacists spending enough time talking to patients which was 42.7%. This depicts to an extent the degree to which pharmacists in the facility offer drug information services to patients. This could be due to want of time as a result of other patients waiting to refill their prescriptions or obtain one product or service. Adequate time taken to communicate with patients is vital and offers an opportunity for the patient not only to understand the information but also to contribute as communication should be a two-way process in patient counseling. The foundational principle for designing patient education services to enhance medication safety is to engage patients as active partners in their care.[23,24] To involve patients effectively, they should be encouraged to inquire about the medicines they are receiving.[21]
Staffing, work pressure, and pace
The ailing points in this safety culture composite were “Staff having an adequate break during their shift” (34.1%), “having enough staff to handle workload” (12.1%), and “Distractions that make it difficult for staff to work accurately” (7.3%). The composite had a 26.4% overall positive score. More than half of respondents (53.1%) said that they feel rushed while processing prescriptions. The concept of feeling rushed during prescription processing opens the door for errors to occur. Work overload exposes staff to intense pressure and stress, fostering the likelihood of making errors. Understaffing is noted to affect patient safety within a structure-process-outcomes framework.[17] Ensuring adequate break time, such as tea breaks, is crucial for revitalizing staff both physically and mentally, contributing to improved performance. Humans inherently have a limited attention span, can focus on only a few things at once, and are susceptible to distractions and interruptions.
Communication about prescriptions across shifts, communication about mistakes, and response to mistakes
Respondents did not have an average (40.7%) positive opinion on “communication about prescriptions.” In particular, the transmission of information regarding problematic prescriptions was ineffective between shifts. There were unclear expectations concerning the exchange of crucial prescription information across shifts, and insufficient standard procedures for communicating prescription details. These communication deficiencies can significantly jeopardize patient safety.[21] Inadequate information transfer and faulty communication pose a potential threat to patient safety.[25]
Organizational learning continuous improvement
This composite had a positive opinion a bit greater than average (56.1%) from the respondents. This positive opinion on this composite is lesser than the opinions of personnel of a pharmacy in a Nigerian tertiary hospital in the South-South with a positive response of 84.0%.[14] About two items had positive responses greater than half –“when a mistake happens, we try to figure out what problems in the work process led to the mistake” (62.1%), “When the same mistake keeps happening, we change the way we do things” (59.8%). The sore item was whether “mistakes have led to positive changes in the pharmacy” (46.3%). It is essential to recognize that the most significant impact on safety and quality improvement is typically achieved locally when an institution incorporates patient safety incident reporting into a continuous system of safety and quality improvement.[21]
Documenting mistakes
It was observed that documentation of mistakes culture by pharmacy personnel had below a third (30.1%) – overall positive response. Irrespective of the situation, whether potential or actual mistakes reach the patient or not, it is crucial to document and discuss all errors. This process helps establish a comprehensive database that can be utilized for internal audits of service delivery processes, aiming to identify and rectify avoidable mistakes.
Overall rating of pharmacy on patient safety
On this item, an overall positive response of 62.2% was recorded. Hence, it is clear that much work is still required to put the pharmacy and pharmacy staff in conditions that would enhance patient safety culture.
CONCLUSION
The respondents provided a relatively satisfactory positive rating for the overall perceptions of patient safety, indicating a strong emphasis on patient safety. However, the culture of documenting mistakes in this pharmacy was identified as lacking. In the end, respondents gave an overall positive rating of 62.2% for patient safety in this pharmacy, which is commendable. Nevertheless, the final rating suggests that there is still room for improvement in the safety culture within this pharmacy.
Acknowledgment
We the authors appreciate the cooperation of all respondents, heads of the Pharmacy Department of the Teaching Hospital Complex.
Ethical approval
The Institutional Review Board gave a verbal consent for the study. The authors certify that they obtained consent from all respondents.
Declaration of patient consent
Patient’s consent was not required, as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: None.
References
- Patient safety. Available from: https://www.who.int/patientsafety/en/2019 [Last accessed on 2023 Aug 07]
- [Google Scholar]
- Evaluation of patient safety culture in community pharmacies. J Patient Saf. 2020;16:e18-e24. doi: 10.1097/PTS.0000000000000245
- [CrossRef] [PubMed] [Google Scholar]
- Clinical pharmacy services, hospital pharmacy staffing, and medication errors in United States hospitals. Pharmacotherapy. 2002;22:134-147. doi: 10.1592/phco.22.3.134.33551
- [CrossRef] [PubMed] [Google Scholar]
- Effects of computerized physician order entry and clinical decision support systems on medication safety. Arch Intern Med. 2003;163:1409-1416. doi: 10.1001/archinte.163.12.1409
- [CrossRef] [PubMed] [Google Scholar]
- Potential risks and prevention, part 4: Reports of significant adverse drug events. Am J Health Syst Pharm. 2001;58:1406-1412. doi: 10.1093/ajhp/58.15.1406
- [CrossRef] [PubMed] [Google Scholar]
- Role of the pharmacist in reducing healthcare costs: Current insights. Integr Pharm Res Pract. 2017;6:37-46. doi: 10.2147/IPRP.S108047
- [CrossRef] [PubMed] [Google Scholar]
- Pharmaceutical care in community pharmacies: Practice and research in the US. Ann Pharmacother. 2006;40:1400-1406. doi: 10.1345/aph.1G545
- [CrossRef] [PubMed] [Google Scholar]
- The role of the pharmacist in the health care system In: Report of a WHO consultative group 1994. Geneva, Switzerland: World Health Organization; 1994.
- [Google Scholar]
- Community pharmacy survey on patient safety culture. 2012. Preliminary Comparative results. Available from: http://www.Ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/pharmacy/2012/index.html [Last accessed on 2023 Oct 10]
- [Google Scholar]
- Evaluation of patient safety culture among Malaysian retail pharmacists: Results of a self-reported survey. Patient Prefer Adherence. 2016;10:1317-1325. doi: 10.2147/PPA.S111537
- [CrossRef] [PubMed] [Google Scholar]
- Safety culture in a pharmacy setting using a pharmacy survey on patient safety culture: A cross-sectional study in China. BMJ Open. 2014;4:e004904. doi: 10.1136/bmjopen-2014-004904
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of patient safety culture: A nationwide survey of community pharmacists in Kuwait. BMC Health Serv Res. 2018;18:884. doi: 10.1186/s12913-018-3662-0
- [CrossRef] [PubMed] [Google Scholar]
- Measuring patient safety culture in Taiwan using the hospital survey on patient safety culture (HSOPSC) BMC Health Serv Res. 2010;10(1):152. doi: 10.1186/1472-6963-10-152
- [CrossRef] [PubMed] [Google Scholar]
- Pharmacy patient safety: 1. Evaluation of pharmacy patient safety culture in a tertiary hospital in Bayelsa State, Nigeria. Sch Acad J Pharm. 2015;4(2):108-116.
- [CrossRef] [Google Scholar]
- Patient safety In: Principles and practice. New York: Springer Publishing Company; 2004. p. :10012-13955.
- [Google Scholar]
- Lack of communication is root of errors. 2003. Research findings presented at AHRQ media briefing. Available from: http://www.reuters.com/newsarticle [Last accessed on 2024 Feb 07]
- [Google Scholar]
- Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiol Scand. 2009;53(2):143-151. doi: 10.1111/j.1399-6576.2008.01717.x
- [CrossRef] [PubMed] [Google Scholar]
- To err is human - Building a safer health system Washington, DC: Rapport Institute of Medicine, National Academy Press; 2000. p. :23.
- [Google Scholar]
- Meta-analysis of teamwork processes: Tests of a multidimensional model and relationships with team effectiveness criteria. Pers Psychol. 2008;61(2):273-307.
- [CrossRef] [Google Scholar]
- Creation of a better medication safety culture in Europe: Building up safe medication practices France: Council of Europe; 2006.
- [Google Scholar]
- IHI. 2012. Available from: http://www.ihi.org/resources/pages/changes/developacultureofsafety.aspx [Last accessed on 2024 Feb 07]
- [Google Scholar]
- ISMP medication safety self-assessment for hospitals. 2004. Available from: http://www.ismp.org/selfassessments/hospital/200 [Last accessed on 2023 Nov 12]
- [Google Scholar]
- Medication safety self-assessment for community/ambulatory pharmacy. Available from: http://www.ismp.org/selfassessments/book.pdf [Last accessed on 2006 Nov 12]
- [Google Scholar]
- From a culture of safety to a culture of excellence: The business of health care. In: A Journal of Innovative Management Collection. Salem, NH: Goal/QPC; 2002.
- [Google Scholar]







