Translate this page into:
Hyperosmolar hyperglycemic state presenting as transient global aphasia
*Corresponding author: Harish Kasarabada, MD Department of Internal Medicine, Army Hospital R and R, New Delhi, India. kasarabadaharish@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kasarabada H, Singh D. Hyperosmolar hyperglycemic state presenting as transient global aphasia. Am J Pharmacother Pharm Sci 2023;016.
Abstract
Hyperosmolar hyperglycemic state (HHS) is an emergency condition characterized by severe dehydration secondary to uncontrolled hyperglycemic state in the absence of ketoacidosis. HHS can present with a variety of neurological symptoms including encephalopathy and seizures. In this report, we present a case of acute-onset transient global aphasia in a 65-year-old male with chronic poor glycemic control. Post-evaluation, we establish the etiology of transient global aphasia as HHS in which patient had complete recovery of symptoms following normalization of blood glucose levels.
Keywords
Hyperosmolar hyperglycemic state
Encephalopathy
Stroke
Electroencephalogram
Aphasia
INTRODUCTION
Hyperosmolar hyperglycemic state (HHS) is an emergency characterized by severe dehydration secondary to an uncontrolled hyperglycemic state in the absence of ketoacidosis. The basic pathophysiology is deficiency of insulin and excess of counter regulatory hormones. It accounts for around 10 times higher mortality in comparison with diabetic ketoacidosis.[1] The diagnosis of HHS is made by high blood glucose levels usually more than 600 milligrams/deciliter (mg/dL) in a setting of known diabetes. In addition, features include dehydration, glycosuria, and serum osmolality more than 300 milliosmoles/kilogram (mosm/kg) (Normal value – 285–295 mosm/ kg).[2] HHS can present with variety of neurological manifestations including encephalopathy, seizures, movement disorders, and rarely with stroke. The pathophysiology behind movement disorders such as chorea or hemiballismus is ischemia secondary to uncontrolled hyperglycemia in contralateral striate arteries which are branches of middle cerebral artery (MCA) which results in abnormal inhibition of caudate and putamen pathways leading hyperkinetic movements.[3] The accepted mechanism of seizures is that, in HHS, there is inhibition of Krebs cycle resulting in increased levels of gamma-aminobutyric acid leading to decreased seizure threshold.[4] The reason for encephalopathy is usually attributed secondary to infections as a result of longstanding uncontrolled hyperglycemic state.[3] Aphasia is a language disorder and is classified by the location of the brain lesion and the resulting symptoms. Broca’s aphasia is characterized by loss of the ability to speak, but with relatively preserved comprehension. The anterior region of the brain, including the inferior frontal gyrus in the dominant hemisphere, is associated with Broca’s aphasia. Wernicke’s aphasia has preserved fluency with poor comprehension. Wernicke’s aphasia usually results from a lesion in the posterior area of the superior temporal gyrus of the dominant hemisphere. In global aphasia, both fluency and comprehension are severely impaired, and the common sites of lesions are in the brain areas surrounding the MCA.[5] HHS presenting as transient global aphasia is rare; in view of the same, we report this case of transient reversible global aphasia secondary to HHS.
CASE REPORT
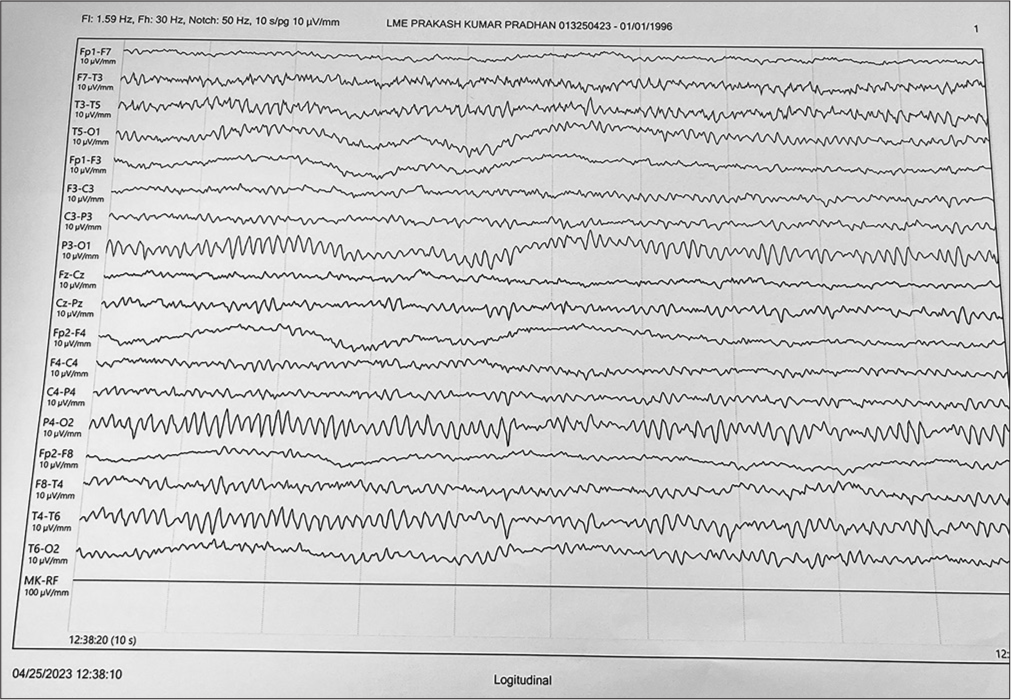
AA is a 65-year-old male, known diabetic (Type II) for 10 years on oral anti-diabetic drugs (Glimepiride 2 mg daily and Metformin 1 g twice daily). He had a history of poor medication compliance and medical follow-up. He became symptomatic with acute onset aphasia with impaired comprehension and fluency; however, at the time of onset, he had history of communication with gestures which were lost progressively over a period of 6 h. He reported to hospital after 8 h of onset of symptoms. On arrival, his vital signs were normal and general examination revealed signs of dehydration. His central nervous system examination revealed global aphasia with Glasgow coma scale (GCS) of 9/15 (Eye4, Verbalmute, Motor5). His GCS was closely monitored and further drop below 8 would have warranted elective intubation to prevent aspiration pneumonia. However, the rest of the systemic examination was within normal limits, provisional diagnosis of stroke was made. His National Institutes of Health Stroke Scale was 9 (with scores between 5 and 15 considered moderate-grade stroke) and random blood glucose at time of presentation was 910 mg/dL. He underwent magnetic resonance imaging of brain which showed no features of acute infarct. Simultaneously, he was started with fluid support, along with insulin infusion; serum osmolality calculated using Dorwart and Chalmers formula revealed 318 mosm/kg. He was diagnosed with HHS and continued aggressive fluid therapy and insulin infusion. Baseline diagnostic tests such as complete blood counts, chest X-ray, and urine microscopic examination were done to rule out any evidence of infection and were within normal limits. His bedside electroencephalogram (EEG) revealed diffuse slow delta waves in both cerebral hemispheres [Figure 1]. After 6 h of management, he had good urine output with blood glucose values below 200 mg/dL and serum osmolality 288 mosm/kg. The patient had complete recovery from aphasia and communicated with good comprehension, fluency, and repeating phrases. His repeat EEG following complete recovery (48 h post-admission) was normal [Figure 2]. He was continued on insulin infusion for 24 h and was discharged from hospital after 2 days after normalization of blood glucose and was counseled on drug compliance and regular medical follow-up.

- Electroencephalogram showing diffuse slow delta waves.
- Normal electroencephalogram following normalization of blood glucose.
DISCUSSION
HHS can present with various neurological symptoms including encephalopathy and seizures. However, aphasia is very rare; here, in this case, we present reversible transient global aphasia secondary to HHS. The pathophysiology of HHS leading to transient aphasia is not fully understood; however, widely accepted theory is glucose-induced reactive oxygen species lead to lipid peroxidation, protein carbonylation, and DNA damage, thereby producing nuclear factor-κB-mediated vascular inflammation.[6] This, in turn, leads to production of nitric oxide, finally resulting in decreased cerebral perfusion. HHS presenting as global aphasia is extremely rare as it requires uncontrolled high blood glucose over a long period to reduce cerebral perfusion for the entire MCA territory circulation to be compromised. However, to define how long uncontrolled blood glucose can lead to aphasia is debatable and requires further studies to establish the time period leading to neurological symptoms. In our case also, the patient was noncompliant with his medications and was lost to follow-up. At presentation, he had blood sugar of 910 mg/dL with preserved sensorium, which implies that he had poor glycemic control over a long period which led to presentation of global aphasia secondary to HHS. The duration of chronic hyperglycemia to develop neurological symptoms cannot be well-defined and requires an individualized approach to define. Although, HHS is known to mimic stroke, neuroimaging should be performed to rule out acute stroke since both pathologies can occur simultaneously. In this case with normal neuroimaging, the diagnosis of HHS presenting with global aphasia was established. EEG was done since HHS can lead to seizures. EEG showed slowing of electrical activity as evident by slow delta waves with no epileptiform discharges. This pattern of EEG can be seen secondary to chronic uncontrolled hyperglycemia and in conditions such as metabolic encephalopathy;[7] however, patient’s metabolic parameters such as urea, creatinine, and electrolytes were within normal limits. He was managed with aggressive fluid support once renal function tests and echocardiography results were within normal limit. Synergistic effects of insulin and fluid therapy led to normalization of blood glucose levels. Once blood glucose fell below 200 mg/dL, the patient recovered fully from aphasia with normal comprehension and fluency. To rule out HHS as the cause of the transient global aphasia, repeat EEG was performed which revealed normal study.
CONCLUSION
HHS presenting as transient global aphasia is rare. We report a case of transient reversible global aphasia secondary to HHS involving a patient with poor history of medication compliance and medical follow-up visits. Our patient made full medical recovery following normalization of blood glucose levels.
Declaration of patient consent
Patient’s consent was not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
None.
References
- Diabetic ketoacidosis and hyperglycemic hyperosmolar syndrome. Diabetes Spectr. 2002;15:28-36. doi:10.2337/diaspect.15.1.28
- [CrossRef] [Google Scholar]
- Diabetic ketoacidosis and hyperglycemic hyperosmolar nonketotic syndrome. Endocrinol Metab Clin North Am. 2000;29:683-705. doi:10.1016/s0889-8529(05)70159-6
- [CrossRef] [PubMed] [Google Scholar]
- Spectrum of hyperosmolar hyperglycaemic state in neurology practice. Indian J Med Res. 2017;146(Suppl 2):S1-S7. doi:10.4103/ijmr.IJMR_57_15
- [CrossRef] [PubMed] [Google Scholar]
- Focal seizures and non-ketotic hyperglycaemia. J Neurol Neurosurg Psychiatry. 1992;55:195-197. doi:10.1136/jnnp.55.3.195
- [CrossRef] [PubMed] [Google Scholar]
- Aphasia and other language disorders. Front Neurol Neurosci. 2012;30:41-45. doi:10.1159/000333402
- [CrossRef] [PubMed] [Google Scholar]
- Insulin inhibits intranuclear nuclear factor. ?B and stimulates IkappaB in mononuclear cells in obese subjects: Evidence for an anti-inflammatory effect? J Clin Endocrinol Metab. 2001;86:3257-3265. doi:10.1210/jcem.86.7.7623
- [CrossRef] [PubMed] [Google Scholar]
- Expressive aphasia as the manifestation of hyperglycemic crisis in Type 2 diabetes. Korean J Intern Med. 2016;31:1187-1190. doi:10.3904/kjim.2014.379
- [CrossRef] [PubMed] [Google Scholar]






