Translate this page into:
Prevention better than cure: expanding on pharmacists’ role in prescription opioid overdose and addiction management
*Corresponding author: Otito Frances Iwuchukwu, RPh, MA, PhD Department of Pharmaceutical Sciences, School of Pharmacy and Health Sciences, Fairleigh Dickinson University, Florham Park, New Jersey, United States. iwuchuof@fdu.edu
-
Received: ,
Accepted: ,
How to cite this article: Iwuchukwu OF, Kim D. Prevention better than cure: expanding on pharmacists’ role in prescription opioid overdose and addiction management. Am J Pharmacother Pharm Sci 2023;022.
Abstract
As prescription opioid misuse and abuse increases in prevalence, pharmacists continue to be in frontlines of prevention and therapeutic management. Pharmacists as public health practitioners should be aware of new and relevant paradigms of substance abuse research and prevention and how they can further contribute to mitigation of opioid and other substance use disorders (SUDs). Screening, brief intervention, and referral to treatment (SBIRT) is a prevention tool that has been used to identify, reduce and misuse, abuse, and dependence on substances, including drugs and alcohol. The screening and brief intervention aspects of SBIRT have been shown to be adaptable across multiple health-care settings. Techniques to conduct applicable stages of SBIRT can be learned and used by pharmacists across multiple practice areas as they engage with the public. SBIRT can be used in conjunction or as a supplementary tool to other prevention and management strategies such as the use of prescription drug monitoring programs and naloxone prescription and distribution. We make a case that pharmacists, particularly those in the community setting, who act as the entry points for many patient engagement encounters, can incorporate SBIRT into their counseling and medication therapy management workflows. As pharmacists continue the move toward codifying provider status, their expertise along with expansion of services, such as the application of SBIRT called for in this article, should be continually leveraged to increase access to treatment and services for at-risk patients with SUDs.
Keywords
Opiod use disorder
Screening
Intervention
Referral
Pharmacist
Interdisciplinary
INTRODUCTION
The magnitude of the prevalence of prescription opioid abuse and attendant opioid/substance use disorder (SUD) is best exemplified using population data. In 2021, the Centers for Disease Control and Prevention (CDC) reported a total of 91,799 overdose deaths in the United States (US) which is up 31% from 2019.[1] Three quarters of reported deaths involved opioids. The 2021 data also showed that more than 9.7 million people in the US, aged 12 and older, misused opioids, including prescription opioids and heroin.[2] Although the number of people with a diagnosed opioid use disorder (OUD) fell for the 1st time in that year,[2] the numbers are still reflective of a SUD crisis.
Many health-care practitioners (HCPs) now find themselves on the frontlines of two crises – the COVID-19 pandemic and opioid misuse. As such, their services and expertise could and should be continually leveraged to increase access to treatments and services for at-risk patients, especially those with SUDs.
Pharmacists are drug experts who are well versed in the pharmacology and mechanism of action of the medications used in medication-assisted treatment and emergency treatment of opioid overdose. Pharmacists are also essential members of the health-care team who could serve as a critical line of defense against the SUD crisis by engaging in modalities involved in prevention and treatment of OUD and overdose.[3,4] However, there is paucity of knowledge regarding the paradigms of substance abuse research and prevention and how pharmacists can further contribute to mitigating SUDs. Emergency treatment paradigms involving access to naloxone, or other institutionalized practices involving opioid stewardship monitoring and prescription drug monitoring programs (PDMP) are not the only roles that pharmacists can play in stemming this enormous public health issue.
The utility of PDMPs as a monitoring tool cannot be overstated seeing that pharmacists are only beginning to scratch the surface of their optimal use. However, we believe that pharmacists as highly trusted health-care professionals can also play a role in the use of prevention strategies.
In this review, we focus on one such strategy; screening, brief intervention, and referral to treatment (SBIRT), an evidence-based public health approach to substance abuse prevention and treatment. It has been shown that SBIRT can be safely incorporated into the patient care counseling process in community[5] or ambulatory care settings.[6] As we move rapidly toward codifying provider status, we make the case for more pharmacist involvement in establishing prevention and early intervention approaches such as SBIRT. We believe that techniques to conduct applicable stages of SBIRT can be learned and used by pharmacists across multiple practice areas as they engage with the public.
PREVENTION EFFORTS AND EARLY INTERVENTION FOR SUDS
A comprehensive approach is needed to manage SUDs as behavioral problems of increasing public health magnitude. Such an approach must include prevention as a key part of an overall continuum of care that includes treatment and recovery [Figure 1].
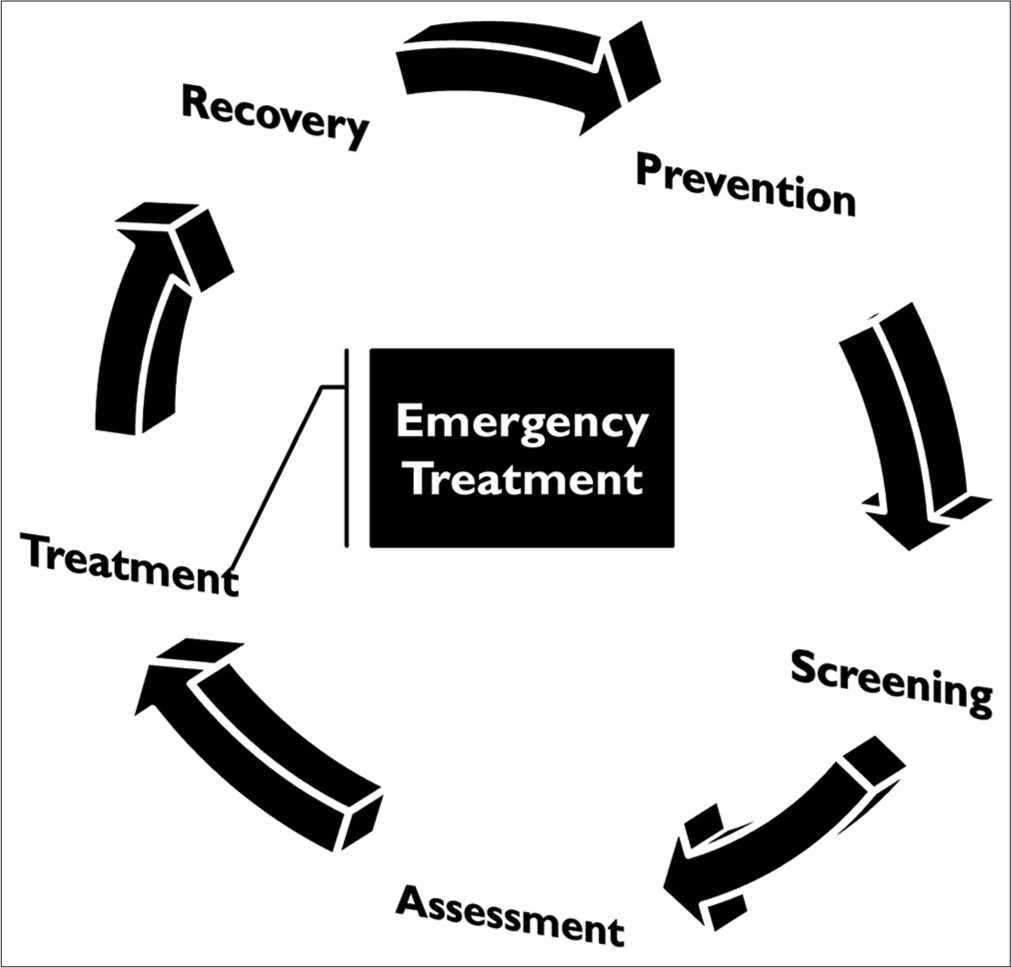
- A representative summary lifecycle from prevention through recovery for substance use disorder management.
Prevention is the first step in delaying both onset and progression of SUDs.[7] Successful prevention efforts require a community- and public health-based approach and should address risk and protective factors relevant to the issue at hand and the populations to be reached. These efforts should take place at the appropriate time, place, and setting, use standardized instruments and protocols, and track measurable skills and goals.[7] HCPs, including pharmacists, must recognize that prevention involves more than discouraging use. Rather, it includes proactive efforts to prevent the negative consequences of drug use as well as to prevent risky use from progression to full-blown substance dependence.
Although many models and approaches for substance abuse prevention exist, not all take an integrated approach to bridging the gap between prevention and treatment efforts.[8]
A validated prevention model that serves as such a bridge is the use of the SBIRT model. This is an approach defined as “a comprehensive integrated public health approach to provide universal screening, secondary prevention, and timely referral (and/or treatment) for individuals with SUDs” This model provides a needed and, in many cases, necessary intersection between prevention and treatment of SUDs. The premise is to effectively target people not yet meeting SUD diagnosis and treatment criteria but who may still place themselves (and others) at risk for harm due to risky substance use.
A key strength to the SBIRT model is universal screening [Figure 2]. This important step has the singular aim of screening all patients irrespective of identified disorders. This universality allows HCPs in a variety of settings to address certain likely behavioral health problems even if patients are not actively seeking interventions or treatment.
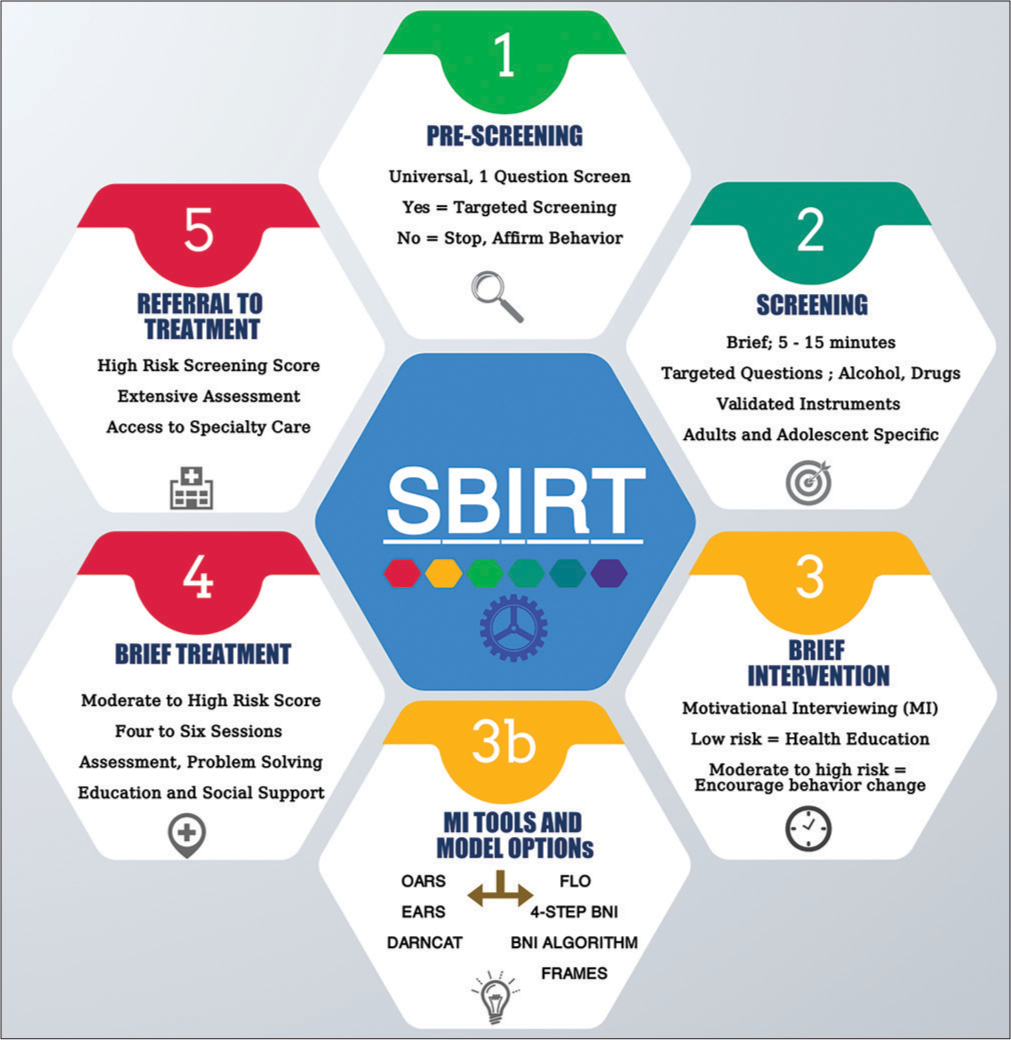
- The steps in the screening, brief intervention (BI), and referral to treatment process. A universal prescreening is inserted before the screening step and the BI step is broken down to focus on various frameworks used in motivational interviewing as a core component in BIs.
A BRIEF OVERVIEW OF SBIRT
Screening (S)
The first step in SBIRT model [Figure 2] begins with the introduction of routine, systematic screening at medical facilities, and other community settings, such as pharmacies, where patients at risk for SUDs may come for medical help.[9] This “screening” is not diagnostic, but rather a process of identifying patients with possible substance misuse and determining a future course of action. The screening provides HCPs with the opportunity to begin discussions with patients about substance use and to provide intervention if required. Screening serves an initial low-cost and low effort triage point. Screening should be brief taking no longer than 5–10 min so that HCPs can continue to fulfill other ancillary responsibilities. Screening is done using validated instruments for purpose and intended population, since adolescents may require different screening instruments.[10] Examples of screening tools for use in SUDs can be found on a dedicated page on the National Institute for Drug Abuse website (nida.nih.gov/nidamed-medical-health-professionals/screening-tools-resources/chart-screening-tools). This website includes a helpful table to help HCPs select the most appropriate tools for any one patient.
For any of these fit-for-purpose instruments, patients are scored based on the scoring system for each tool. Low scores typically indicate little to no risky behavior which may likely require no interventions. However, low scoring patients can still benefit from universal prevention education to reinforce positive behaviors. Patients with moderate and higher screening scores may require brief interventions and further referrals. Screening can be repeated at various intervals, such as during annual visits where needed, to document longitudinal changes in patient progress. Pharmacists are suitably poised to conduct these screenings as many of them are the most proximal point-of-access HCPs over such time periods.
Brief intervention (BI)
BI includes time limited (≤5 min) efforts to provide information and intervention(s) based on motivational interview conversations. The central element of a BI involves motivational interviewing techniques, where the HCP serves as a facilitator in helping persons explore their motivation to change.[11,12] This interaction should not be a provider-centered approach but should instead focus on increasing patients’ insight and awareness about risky substance use and behavioral changes. Pharmacists should be aware that BIs usually done using a visual chart and are conducted only with patient consent, fully invoking the individual’s autonomy for decisions on change readiness.[13] [Figure 3] provides key steps involved in BI. A BI should ideally be provided at the same site and place where screening occurs. Many frameworks and models for BI have been validated. Motivational interventions in emergency department and public health settings reportedly reduced overdose risk behaviors and nonmedical use of opioids.[14,15] A BI between HCPs and persons at moderate or higher risk has been shown to be both cost effective and time efficient.[9]
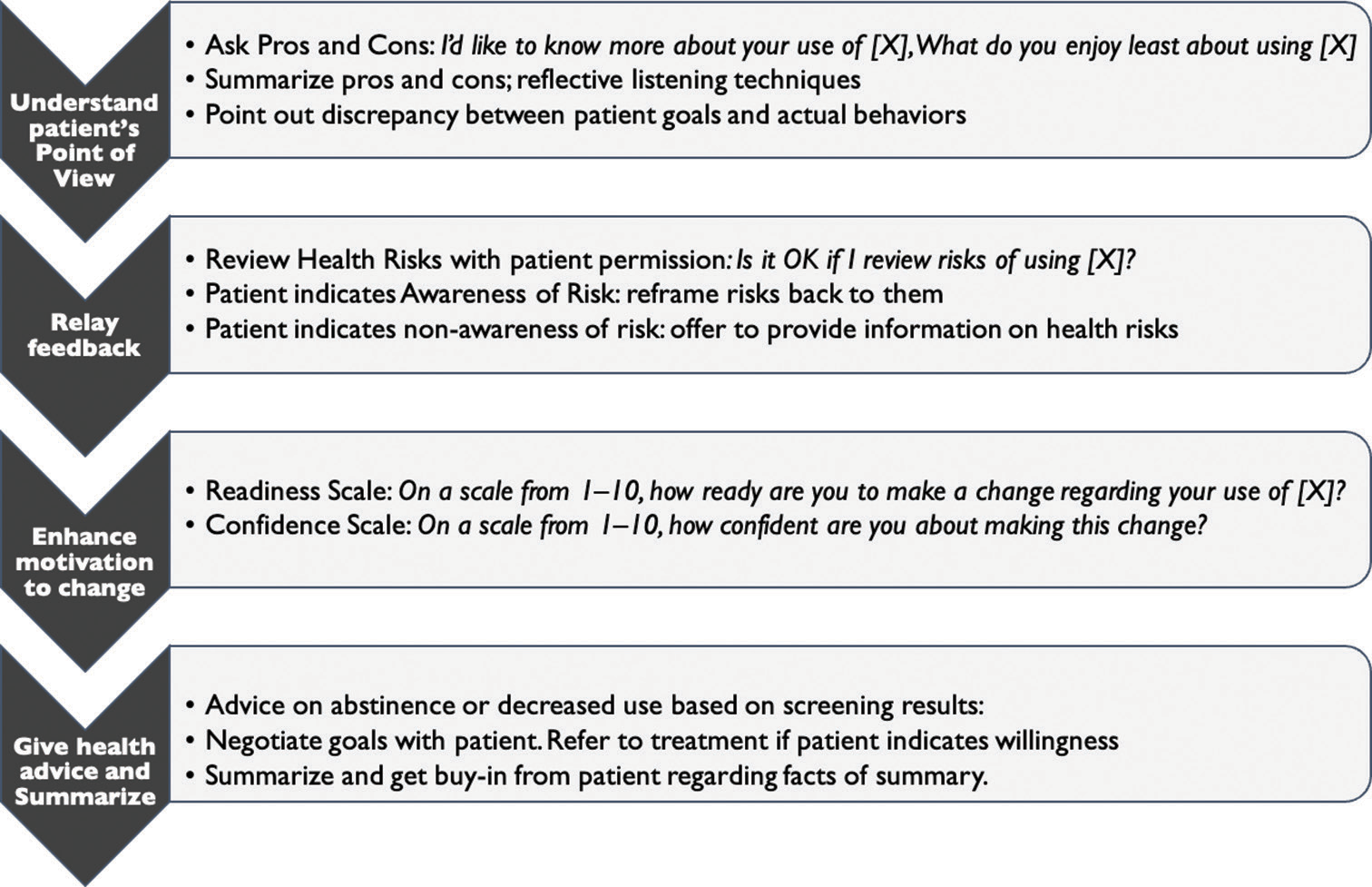
- Sample steps for a brief intervention as conducted using a brief negotiated interview algorithmic approach.
Referral to treatment (RT)
After a consented BI, patients identified as needing more intensive intervention are often referred for Brief and Specialty Treatment, an SBIRT step called RT. Brief treatment is typically a specialty outpatient treatment model unlike longer term residential specialty care. This aspect of SBIRT is out of pharmacists’ purview and professional scope of practice. However, while pharmacists may not be able to conduct an RT, they can still provide information on outpatient treatment centers to patients and facilitate patient engagement with seeking treatment.[4] It may be beneficial for the pharmacists to have the list of national and local groups and organizations that they can connect the patients. RT should not be a hindrance to developing other SBI activities which have been shown to offer huge benefits separate from referral.
ADVANTAGES OF SBIRT
SBIRT allows for increased/better uptake by busy HCP of reliable data from validated screening tools. These data can be integrated into patients’ electronic health record to enhance multidisciplinary care. SBIRT is designed to be conducted quickly and with little specialized training, much less compared to other behavioral health and counseling techniques. Along with the reduced burden on time and prior training, the strong referral component of SBIRT assures that patients are connected to the appropriate specialty care.
PHARMACISTS AND SBIRT TRAINING AND USE – THE CLINICAL AND TRANSLATIONAL EVIDENCE
Prescription opioids are one of the most prevalent categories of illicit drug use in peoples aged 12 and older (3.3% misuse in the past month in 2021).[2] As persons in charge of ensuring optimal medication therapy management, screening and offering consented BI should be incorporated into one of the pharmacist’s responsibilities and responsibilities along with offering counseling and education for naïve and chronic opioid users. The evidence for BI clearly indicates that even short conversations with an HCP can help reduce both the risk of and progression to SUDs.[8]
As a result, there are calls for SBIRT to be taught early in HCPs education and training and to be offered as part of mandated continuing education. Since 2003, the substance abuse and mental health services administration has invested millions of dollars in grant funding for SBIRT programs in the following listed categories – 12 targeted capacity expansion campus screening and brief intervention (SBI) grants, and 14 SBIRT medical professionals training grants (www.samhsa.gov/sbirt/grantees).
Areas of strength and implementation for pharmacists
The adaptability and ease of use of the SBIRT ensures that it can be flexibly applied across multiple health-care settings. SBIRT has been adapted for use in the emergency room, office and clinic-based practices, and various community settings.[16-18]
Community pharmacies can be one of the many settings where SBIRT may be successfully applied. A framework of care study for screening, education, and possible RT for opioid misuse in a community pharmacy setting[19] posited that the various elements of SBIRT could be interwoven into a busy community pharmacist’s workflow. Figure 4 presents a simplified view of where SBIRT can be integrated within the community pharmacists’ work model. They also suggested that community pharmacies be included as an entry point for patient engagement before hand-off to other specialty practitioners.
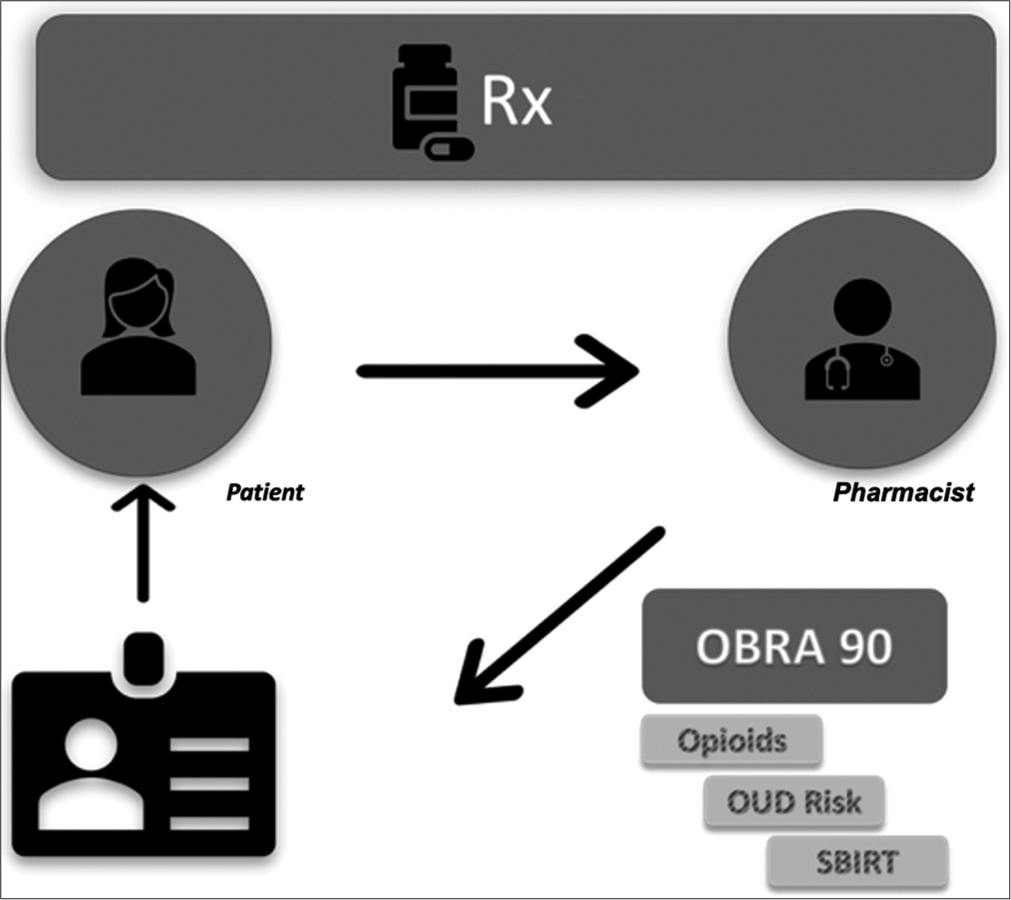
- A sample representation depicting where screening, brief intervention, and referral to treatment can be incorporated under an OBRA ‘90 mandated pharmacist counseling and/or medication therapy management process.
The feasibility of implementing screening and BI for opioid outcomes was tested in an open-label single-arm implementation effectiveness study by Nielsen et al.[20] Pharmacists’ self-assessment of knowledge and confidence in identifying unmanaged pain, depression, and opioid dependence were measured before and after implementation of a software-driven screening system. They found that pharmacists’ confidence in identifying and responding to opioid-related problems from baseline to follow-up increased significantly across several domains, although with room for more scope to further increase confidence when responding to opioid-related problems.[20]
Another study by Strand et al.[21] evaluated the utility of an opioid misuse prevention kit which incorporated as a critical component, the validated opioid risk tool (ORT) developed for OUD screenings. Pharmacists used the scoring system of ORT to stratify the level of intervention provided to patients. The study found that pharmacists preferred having an objective measurement of potential of opioid misuse such as ORT compared to relying only on their professional judgment.
What is being done to prepare current and future pharmacists to embrace SBIRT?
Because SBIRT follows a research-education-practice model, it is essential that health care and pharmacy researchers find a way to bridge the gap between knowing what the research tells us, to educating current and future pharmacy practitioners, to establishing models for frictionless implementation. When considering SBIRT in its entirety, including the RT component, we see its strong interdisciplinary linkage. As such, it is crucial to train and enable pharmacists within this framework using interprofessional education modalities,[22,23] such as was done for a rural family medicine clinic.[6]
For training, it is essential that everyone be taught to the same competency level to enable a more standardized approach in implementation and use. The study by Pringle et al.[24] reported the development and evaluation of two SBIRT proficiency checklists for the use across institutions to assess SBIRT skills in both simulated and clinical encounters, with the goal being for easy integration as standard instruments in a wide variety of training settings. Proficiency and competency checklists can go a long way in helping standardize SBIRT trainings.
Some studies have examined pharmacists’ and patients’ perception of acceptability, uptake and utilization of interventions such as SBIRT in the community settings, and found that counseling interventions as well as the use of PDMPs have increased.[25-27] To further support implementation of SBIRT into community practice setting, studies such as those by Fatani et al. who used a modified Delphi approach in the development of a toolkit inform us that SBIRT model can be integrated into the community practice setting.[28]
OTHER OUD PREVENTION AND MANAGEMENT STRATEGIES
While we have focused this review on the advantages and utility of SBIRT as a SUD prevention approach, SBIRT by itself cannot curb the current epidemic of substance misuse and abuse. In this section, we briefly discuss other pharmacist-led or pharmacist-partnered approaches and interventions for the prevention and management of SUDs.
PDMP utilization by pharmacists
The impact of PDMP has been overall positive, but the extent of the impact variable. When a national survey was administered to physicians at community health centers during the time PDMP was operational in 24 states, it revealed that the implementation of PDMP was associated with decrease in the prescribing of schedule II drugs. This deprescribing was sustained through 24 months.[29] In a retrospective analysis of national data, implementation of PDMP has been found to reduce the number of opioid overdose deaths by 1.12/every 100,000 population after adjustment for the programs that monitored four or more drug schedules and updated data at least weekly.[30] This is a significant finding as the average opioid-related overdose death rate for the 34 states that were included in this analysis was noted as 6.2/100,000 in 2013, risen from 1.4/100,000 in 1999. The PDMP Training and Technical Assistance Center has published the Best Practice checklist, recommending mandated utilization by both prescribers and dispensers.[31] States have taken a variety of steps to implement PDMP. Ohio, for example, has taken radical actions in addressing opioid epidemic, one example being pharmacists mandate in utilizing the patient’s PDMP history before dispensing any new controlled substance prescription.[32]
PDMP overall has positive and unforeseen negative impacts. Between the period before and after the publication of CDC’s Guideline for Prescribing Opioids for Chronic Pain, opioid prescribing was reduced from 7.4% to 6.4% in a cohort of 31,422 primary HCPs serving 17 million people. It is sobering to grasp this reduction in light of continued increase of deaths from heroin and fentanyl overdose.[33] Based on an interview with PDMP staff, law enforcement officials and administrative agency employees in several states, one of the unintended consequences of PDMP implementation was noted to be the rise in heroin use as opioid pain reliever substitute and its related deaths.[34] Pharmacists should be educating the public and the patients on this potential harmful consequence.
Creating and adopting policies and procedures within health systems
Due to the various types of opioid formulations (e.g., parenteral) and the involvement of multiple personnel before the medication reaches the end user, opioid diversion and misuse can be a particular problem within health systems. Health system pharmacies must have strict policies discouraging drug diversion by hospital personnel.[35] Full utilization of the PDMP can ensure proper prescribing and dispensing of opioids within health systems. In addition, pharmacists should participate in the creation of guidelines and protocols that pertain to opioid-related activities.
Community-based interventions
The World Health Organization recognizes OUD as a significant global health burden. Among the several recommended strategies for improvement in access to healthcare, “indigenous medical sectors” are noted as one of the key sectors that can be engaged to improve care for individuals with OUD.[36] We propose that community pharmacies can be a “indigenous medical sectors” that can aid in increased access to professional services for the individuals with OUD. Mental Health First Aid USA is a first aid tool that is offered to individuals who are developing a mental health or substance use challenges. Those who are trained in Mental Health First aid are able to identify and understand individuals who are struggling with substance use challenges and help. In a systemic review of the outcomes of Mental Health First Aid, there was increased knowledge and confidence in assisting a person with mental health and substance use challenges as well as accurate identification of mental illness.[37] Pharmacists can become certified mental health first aid practitioners and trainers and help to bridge the gap in improving access to care.
Independent groups of experts have produced other community-focused patient assessment algorithms to help identify possible opioid misuse/abuse risk and OUD. For example, verification, identification, generalization, interpretation, and legalization is a risk-stratifying system that has factors that add or subtract points toward an overall score. Patients are classified as “low risk” (scores 0–4), “medium risk” (scores 5–9), or “high risk” (scores 10+) based on the presence of these factors (e.g., cash payment). Patients with medium or high risk may require further intervention by the pharmacists, such as requesting the prescriber to forward medical records for review.
Naloxone distribution
Naloxone distribution to any persons likely to witness an opioid overdose is another strategy to address the national opioid epidemic. Pharmacists and pharmacies act as a critical point of naloxone sales, distribution, public education, and individual assessment. Jones et al. have reported a more than a 10-fold increase in the dispensing of naloxone in the US community pharmacies over the period 2010 and 2015.[38] Consistent with the increase in naloxone distribution was seen an increase of 26,463 opioid overdose reversals between 2013 and 2014.[39] These numbers are expected to increase as more data accumulates around this effective overdose prevention and treatment strategy.
CONCLUSION
The SBI aspects of SBIRT have been shown to be adaptable across multiple health-care settings. The feasibility of implementing SBIRT in the community and rural health-care settings, an expansion from urban health-systems, has been tested. Techniques to conduct applicable stages of SBIRT can be learned and used by pharmacists across multiple practice areas. SBIRT is a useful validated tool that can be best used by pharmacists in conjunction or as a supplement to other prevention and management strategies such as the use of PDMPs and naloxone prescription and distribution. As pharmacists continue the move toward codifying provider status, their expertise along with expansion of services such as SBIRT can be leveraged as one pathway to increase access to screening services for at-risk SUD patients.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
None.
References
- Drug overdose deaths. Available from: https://www.cdc.gov/drugoverdose/deaths/index.html [Last accessed on 2023 Jul 04]
- [Google Scholar]
- Key substance use and mental health indicators in the United States: Results from the 2019 national survey on drug use and health. 2020. Available from: https://www.samhsa.gov/data/report/2019-nsduh-annual-national-report [Last accessed on 2023 Jul 04]
- [Google Scholar]
- Pharmacists: On the front lines. Available from: https://www.cdc.gov/drugoverdose/pdf/pharmacists_brochure-a.pdf [Last accessed on 2023 Jul 05]
- [Google Scholar]
- Promising roles for pharmacists in addressing the U.S. opioid crisis. Res Soc Adm Pharm. 2019;15:910-916. doi:10.1016/j.sapharm.2017.12.009
- [CrossRef] [PubMed] [Google Scholar]
- Screening, Brief intervention, and referral to treatment in a retail pharmacy setting: The pharmacist's role in identifying and addressing risk of substance use disorder. J Addict Med. 2019;13:403-407. doi:10.1097/ADM.0000000000000509
- [CrossRef] [PubMed] [Google Scholar]
- Interdisciplinary SBIRT training for pharmacy students in a rural family medicine clinic. JACCP J Am Coll Clin Pharm. 2020;3
- [Google Scholar]
- Committee on Prevention DT and M of SUD in the USAFB on the H of SPI of M. best practices in prevention, screening, diagnosis, and treatment of substance use disorders In: O'Brien C, Oster M, Morden P, eds. Substance use disorders in the U.S. Armed Forces. National Academies Press (US); 2013. Available from: https://www.ncbi.nlm.nih.gov/books/NBK207270 [Last accessed on 2023 Jul 07]
- [Google Scholar]
- Systems-level implementation of screening, brief intervention, and referral to treatment United States: Substance Abuse and Mental Health Services Administration; 2013.
- [Google Scholar]
- Screening, brief intervention, and referral to treatment (SBIRT): Toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7-30. doi:10.1300/J465v28n03
- [CrossRef] [PubMed] [Google Scholar]
- Screening for unhealthy drug use in primary care in adolescents and adults, including pregnant persons: Updated systematic review for the U.S. Preventive services task force. Rockville, MD: Agency for Healthcare Research and Quality; 2020. p. :186.
- [CrossRef] [PubMed] [Google Scholar]
- What is motivational interviewing? Behav Cogn Psychother. 1995;23:325-334. doi:10.1017/S135246580001643X
- [CrossRef] [Google Scholar]
- What is motivational interviewing? The spirit of motivational interviewing. Behav Cogn Psychother. 2019;23:325-334.
- [CrossRef] [Google Scholar]
- Motivational interviewing in health care: Helping patients change behavior. COPD: J Chron Obstruct Pulmon Dis. 2008;5:3. doi:10.1080/15412550802093108
- [CrossRef] [Google Scholar]
- Naloxone for heroin, prescription opioid, and illicitly made fentanyl overdoses: Challenges and innovations responding to a dynamic epidemic. Int J Drug Policy. 2017;46:172-179. doi:10.1016/j.drugpo.2017.06.005
- [CrossRef] [PubMed] [Google Scholar]
- Opioid prescribing in the United States before and after the centers for disease control and prevention's 2016 opioid guideline. Ann Intern Med. 2018;169:367-375. doi:10.7326/M18-1243
- [CrossRef] [PubMed] [Google Scholar]
- Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: A brief review. J Psychoactive Drugs. 2012;44:307-317. doi:10.1080/02791072.2012.720169
- [CrossRef] [PubMed] [Google Scholar]
- Implementing SBIRT (Screening, Brief Intervention and Referral to Treatment) in primary care: Lessons learned from a multi-practice evaluation portfolio. Public Health Rev. 2017;38:31. doi:10.1186/s40985-017-0077-0
- [CrossRef] [PubMed] [Google Scholar]
- Prevention and screening, brief intervention, and referral to treatment for substance use in primary care. Prim Care. 2014;41:185-213. doi:10.1016/j.pop.2014.02.002
- [CrossRef] [PubMed] [Google Scholar]
- Developing a framework of care for opioid medication misuse in community pharmacy. Res Social Adm Pharm. 2016;12:293-301. doi:10.1016/j.sapharm.2015.05.001
- [CrossRef] [PubMed] [Google Scholar]
- Routine opioid outcome monitoring in community pharmacy: Outcomes from an open-label single-arm implementation-effectiveness pilot study. Res Social Adm Pharm. 2020;16:1694-1701. doi:10.1016/j.sapharm.2020.02.009
- [CrossRef] [PubMed] [Google Scholar]
- Moving opioid misuse prevention upstream: A pilot study of community pharmacists screening for opioid misuse risk. Res Social Adm Pharm. 2019;15:1032-1036. doi:10.1016/j.sapharm.2018.07.011
- [CrossRef] [PubMed] [Google Scholar]
- Developing a screening, brief intervention, and referral to treatment (SBIRT) program with multiple health professions programs. J Interprof Care. 2019;33:828-831. doi:10.1080/13561820.2019.1569601
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of screening, brief intervention, and referral to treatment training to interprofessional health-care students. SAGE Open Nurs. 2019;5 doi:10.1177/2377960819834132
- [CrossRef] [PubMed] [Google Scholar]
- Development and evaluation of two instruments for assessing screening, brief intervention, and referral to treatment (SBIRT) competency. Subst Abus. 2017;38:43-47. doi:10.1080/08897077.2016.1152343
- [CrossRef] [PubMed] [Google Scholar]
- The attitudes and practice strategies of community pharmacists towards drug misuse management: A scoping review. J Clin Pharm Ther. 2020;45:430-452. doi:10.1111/jcpt.13100
- [CrossRef] [PubMed] [Google Scholar]
- Pharmacist utilization of prescription opioid misuse interventions: Acceptability among pharmacists and patients. Res Social Adm Pharm. 2019;15:986-991. doi:10.1016/j.sapharm.2019.01.002
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with provision of addiction treatment information by community pharmacists. J Subst Abuse Treat. 2015;52:67-72. doi:10.1016/j.jsat.2014.11.006
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of patient-community pharmacist encounter toolkit regarding substance misuse: Delphi procedure. J Am Pharm Assoc (2003). 2022;62:176-186. doi:10.1016/j.japh.2021.08.018
- [CrossRef] [PubMed] [Google Scholar]
- Prescription drug monitoring programs are associated with sustained reductions in opioid prescribing by physicians. Health Aff (Milwood). 2016;35:1045-1051. doi:10.1377/hlthaff.2015.1673
- [CrossRef] [PubMed] [Google Scholar]
- Implementation of prescription drug monitoring programs associated with reductions in opioid-related death rates. Health Aff (Milwood). 2016;35:1324-1332. doi:10.1377/hlthaff.2015.1496
- [CrossRef] [PubMed] [Google Scholar]
- The best practice checklist the prescription drug monitoring program training and technical assistance center In: The Heller school for social policy and management. United States: The Bureau of Justice Assistance; 2017.
- [Google Scholar]
- Strategies and policies to address the opioid epidemic: A case study of Ohio. J Am Pharm Assoc. 2017;57:S148-S153. doi:10.1016/j.japh.2017.01.001
- [CrossRef] [PubMed] [Google Scholar]
- Opioid prescribing rates in nonmetropolitan and metropolitan counties among primary care providers using an electronic health record system-United States, 2014-2017. MMWR Morb Mortal Wkly Rep. 2019;68:25-30. doi:10.15585/mmwr.mm6802a1
- [CrossRef] [PubMed] [Google Scholar]
- Perceived unintended consequences of prescription drug monitoring programs. Subst Use Misuse. 2018;54:1-5. doi:10.1080/10826084.2018.1491052
- [CrossRef] [PubMed] [Google Scholar]
- The opioid abuse and misuse epidemic: Implications for pharmacists in hospitals and health systems. Am J Health Syst Pharm. 2014;71:1539-1554. doi:10.2146/ajhp140157
- [CrossRef] [PubMed] [Google Scholar]
- Addressing the burden of mental, neurological, and substance use disorders: Key messages from Disease Control Priorities, 3rd edition. Lancet. 2016;387:1672-1685. doi:10.1016/S0140-6736(15)00390-6
- [CrossRef] [PubMed] [Google Scholar]
- Systematic review and meta-analysis of mental health first aid training: Effects on knowledge, stigma, and helping behaviour. PLoS One. 2018;13:e0197102. doi:10.1371/journal.pone.0197102
- [CrossRef] [PubMed] [Google Scholar]
- Increase in Naloxone prescriptions dispensed in US retail pharmacies since 2013. Am J Public Health. 2016;106:689-690. doi:10.2105/AJPH.2016.303062
- [CrossRef] [PubMed] [Google Scholar]
- Opioid overdose prevention programs providing naloxone to laypersons-United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:631-635.
- [Google Scholar]






