Translate this page into:
Leukemoid reaction: A rare complication of severe dengue
*Corresponding author: Harish Kasarabada, Department of Internal Medicine, Army Hospital Research and Referral, Delhi, India. kasarabadaharish@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kasarabada H, Matta M. Leukemoid reaction: A rare complication of severe dengue. Am J Pharmacother Pharm Sci 2024:2.
Abstract
Leukemoid reaction (LR) is characterized by a leukocyte count of over 50000 cells/cubic millimeter with a significant increase in mature neutrophils on peripheral blood smears as a result of reactive causes outside the bone marrow. Dengue infection is a febrile illness caused by one of four serotypes of the dengue virus and is transmitted by a mosquito named Aedes aegypti or Aedes albopictus. We report the first case report of LR in a confirmed case of dengue infection.
Keywords
Leukemoid reaction
Leukocyte alkaline phosphatase
Dengue
Leukocytosis
INTRODUCTION
Leukemoid reaction (LR) is characterized by a leukocyte count of over 50000 cells/cubic millimeter (mm3) with a significant increase in mature neutrophils on peripheral blood smear (PBS) because of reactive causes outside the bone marrow. It is a diagnosis of exclusion after ruling out hematological conditions such as chronic myeloid leukemia (CML), polycythemia, and chronic neutrophilic leukemia (CNL). LR is characterized by an elevated leukocyte alkaline phosphatase (LAP) score, an enzyme present in microsomes of neutrophil bands, myelocytes, and metamyelocytes. The etiology of LR includes infection (disseminated tuberculosis, clostridium difficile colitis, and shigellosis) and malignancies such as lymphomas, sarcoma, melanoma, drug induced (corticosteroids and minocycline), ethylene glycol intoxication, and acute hemolysis.[1] LR secondary to viral infections is very rare with few cases reported.
CASE REPORT
A 45-year-old woman with no previous medical condition presented with chief complaints of fever for a three-day duration. Fever was continuously high associated with chills, rigors, and myalgia. She had no significant contributory history, occupational or personal history. She denied any contact with pets and working in paddy fields. Her systemic clinical examination revealed no abnormality with provisional investigations of leukopenia (3100 cells/mm3) (normal range: 4000–11000/mm3), thrombocytopenia (platelet count: 120000 cells/mm3) (normal range: 150000–450000 cells/mm3), and elevated levels of serum lactate dehydrogenase (LDH) enzyme (986 international units/liter [IU/L], normal range: 140–290 IU/L). She was admitted to the hospital and was managed symptomatically with antipyretics and fluid therapy.
In her diagnostic workup, non-structural antigen-1 by enzyme-linked immunosorbent assay and dengue real-time reverse transcriptase-polymerase chain reaction were positive confirming diagnosis as a case of dengue infection. Following confirmation of the diagnosis of dengue fever, we continued to manage her symptomatically. She was afebrile following 48 hours of admission; however, she developed anicteric hepatitis, features of the capillary leak in the form of ascites, and pleural effusion. On day 6 of her illness, she had an elevated leukocyte count of 22000 cells/mm3 and liver transaminases of more than 1000 IU/L (both alanine and aspartate aminotransferases). Her leukocyte counts further increased to 58000 cells/mm3 within 2 days, and PBS revealed the predominance of neutrophils with both mature and immature forms [Figure 1 (a and b)] with no evidence of toxic granulation, Dohle bodies or cytoplasmic vacuoles. LR was suspected, and as it is a diagnosis of exclusion testing for CML (breakpoint cluster region-Abelson proto-oncogene [BCR-ABL] quantitative analysis), flow cytometry analysis of peripheral blood for any aberrancies was performed. LR diagnosis was confirmed after ruling out all other differentials in the presence of a high LAP score of 200 IU/L (normal: <130 IU/L). She was managed symptomatically with adequate fluid and nutrition support. On her day 12 of illness, the leukocyte count and liver transaminases returned to normal limits, and she was subsequently discharged after complete clinical recovery.
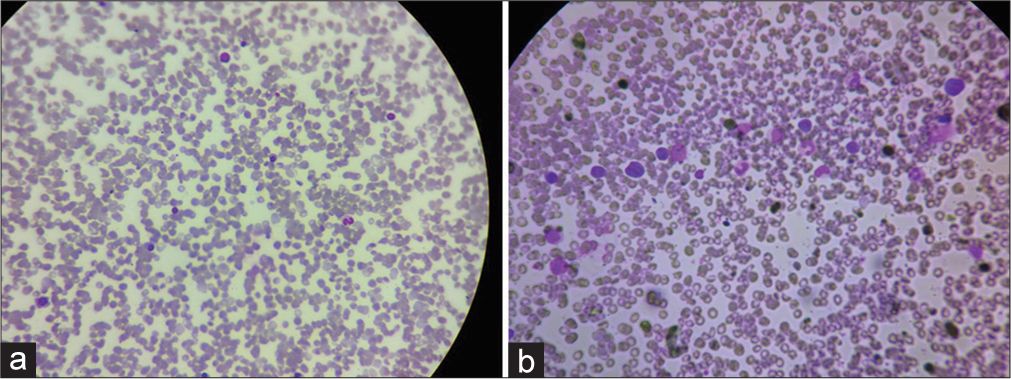
- (a and b) Peripheral blood smear in Giemsa stain at ×400 magnification showing leukocytosis with left shift, predominantly showing immature granulocytes comprising of band forms, metamyelocytes, and myelocytes with increased granules. Occasional nucleated red blood cells are also seen.
DISCUSSION
Dengue infection is a febrile illness caused by one of four serotypes of the dengue virus and is transmitted by a mosquito named Aedes aegypti or Aedes albopictus. The World Health Organization (WHO) revised the classification in 2009 and classified dengue into three categories, namely dengue with warning signs, dengue without warning signs, and severe dengue. Serum levels of LDH at the time of presentation in a confirmed case of dengue can predict severity and act as a prognostic marker.[2] In this case, the patient had an LDH of 986 IU/L (normal value of 140–290 IU/L) by colorimetric analysis, which indicated a high probability of developing warning signs or progressing to severe dengue in due course. With the exception of a few case reports, LR in viral infections is very rare. A similar kind of case was reported where a patient developed LR following chikungunya fever.[3] LR development mechanisms are bone marrow response secondary to increased demand, allergen-driven bone marrow stimulation, and ectopic hematopoiesis due to bone marrow damage.[4] In this case of confirmed dengue, the development of LR happened during the end of the febrile phase followed by normalization of leukocyte count at the end of the critical phase. Moreover, complications of the capillary leak and elevated liver transaminases of more than 1000 U/L (a characteristic feature of severe dengue as per the WHO revised dengue severity classification) coincided with the highest leukocyte count. The probable mechanism of development of LR in this case of confirmed dengue is due to bone marrow stimulation secondary to high viral load. The most important differentials in this case were sepsis (secondary to bacterial infections), CML, and CNL. These differentials were ruled out by performing PBS, flow cytometry, and BCR-ABL quantitative analysis. We continued to treat the case symptomatically, which led to progressive normalization of leukocyte count as well as clinical improvement along with normal liver transaminases at the time of discharge.
CONCLUSION
LR is rare in viral infections. High viral load can lead to increased transient bone marrow activity leading to LR, which is often self-limiting with symptomatic management.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
None.
References
- An update on the etiology and diagnostic evaluation of a leukemoid reaction. Eur J Intern Med. 2006;17:394-398. doi: 10.1016/j.ejim.2006.04.004
- [CrossRef] [PubMed] [Google Scholar]
- Observational study of using lactate dehydrogenase as a prognostic marker in dengue patients. Med J Armed Forces India 2023
- [CrossRef] [Google Scholar]
- Leukemoid reaction in chikungunya fever. J Clin Diagn Res. 2016;10:OD05-OD06. doi: 10.7860/JCDR/2016/18434.7720
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






