Translate this page into:
Mass casualty incident response: Assessment of the level of preparedness among hospital pharmacists
*Corresponding author: Uchenna I. H. Eze, Pharm D, PhD Department of Clinical Pharmacy and Biopharmacy, Olabisi Onabanjo University, Sagamu, Nigeria. ifyeze3000@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Eze UIH, Adebisi OF, Uwaezuoke OJ, et al. Mass casualty incident response: Assessment of the level of preparedness among hospital pharmacists. Am J Pharmacother Pharm Sci 2023;010
Abstract
Objectives:
Mass casualty incidents (MCIs) and outcomes depend on the resources of the admitting institutions and their preparedness, respectively. We assessed the preparedness of hospital pharmacists for MCIs.
Materials and Methods:
A cross-sectional survey was conducted among 132 pharmacists working in hospitals in Ogun State, Southwestern Nigeria, over 1 month, using a 26-item self-administered questionnaire. Data were analyzed using the Statistical Package for the Social Sciences (SPSS, version 21). A Chi-square test was used for further analysis. P <0.05 was considered statistically significant.
Results:
The response rate was 79.5% (105/132). Most respondents were 26–30 years, 31.4%, had been practicing for <10 years, 44.8%, and were female, 59.0%. Overall, 42.9% of the respondents had >400 beds, 66 (62.9%), and 48 (45.7%) had general and pharmacy-specific disaster preparedness plans, respectively. Respondents agreed that the hospital committee consensus determined medications to be stocked, 64 (60.9%) and that disaster plans were mainly for natural disasters, 73 (35.4%). Only 7 (6.6%) respondents practiced mock disaster preparedness. There was a significant association between respondents’ year of practice and response on including disaster events in the institutional plan (χ2 = 95.637, df. = 72, P = 0.033). Most respondents, 95 (90.0%), were positive (mean ± SD: 4.42 ± 0.875) about the need for analgesics during disaster events.
Conclusion:
Preparation for disaster preparedness was suboptimal based on the number of beds, pharmacy-specific disaster preparedness plan, and practice for mock disasters. This calls for immediate awareness to address these shortfalls through orientation, training, and retraining on preparedness for MCIs.
Keywords
Disaster plans
Hospital pharmacy
Mass casualty incidents
Pharmacists
Preparedness
INTRODUCTION
Events that confound the local health-care system, with casualties that overwhelm the locally available resources and capabilities in a short time, are known as mass casualty incidents (MCIs).[1] Forms of MCIs,[2] including the recent COVID-19 pandemic, may occur locally, regionally, or globally. They rely on the admitting institutions’ resources while the outcomes of these incidences depend on an institution’s or community’s preparedness.[1]
According to the United Nations Office for Disaster Risk Reduction Definition, disasters lead to human, material, economic, and environmental losses and impacts.[3] Nigeria is still evolving in its capacity and capability in health-care framework to manage disasters, particularly hospital pharmacists’ preparedness in MCIs.
The number of disasters has increased considerably in the past decade.[4] These incidents claimed the lives of many citizens. In addition, they have left some with permanent disabilities, and disorganized infrastructure and settlement. This fact remains true in Nigeria. The Ebola virus entered Nigeria in July 2014 and was contained 3 months later. Measures taken to achieve this containment include the rapid establishment of an emergency operations center, repurposing advancements, and infrastructure from the WHO and other partners to help find cases and track potential routes of the spread of the Ebola virus disease.[5] Some of these measures were applied to manage the COVID19-pandemic. The index case of COVID-19 in Nigeria was reported on February 27, 2020. Measures to reduce the spread of the COVID-19 virus included staying at home, public health education, handwashing, social distancing, and enforcement of wearing of facemasks.[6]
When disasters occur, hospitals are among the key institutions to manage these conditions as they are seen as a haven where victims seek solace.[7] Hospitals issue emergency care services and are discerned as vital resources for detection, treatment, and follow-up for both physical and psychological care. The main goal is to save as many lives as possible, which requires dedicating limited resources in an adjusted and efficient manner. Disasters have the tendency of causing mass casualties, placing a heavy burden on hospital services, which may inundate the hospital’s resources, staff, space, and supplies, causing uncertainty and inadequacy in the hospital. It is important for hospitals to have well-documented and tested disaster management plans to prepare them to handle unexpected workloads.[8]
Health-care facilities and personnel are critical to disaster response. The effective participation of all key medical service providers within a multidisciplinary team is required for hospital disaster preparedness to be achieved.[9] The preferred framework has been described as “…one in which the established health-care system (hospital administrators and emergency departments, physicians, emergency medical services, community health clinics, pharmacists, and other caregivers) works closely with the public health community (local departments of public health), then explicitly brings the local emergency management agency into the process…,” while the alternative of silo-based independent goals and objectives is ineffective and inefficient.[10] Pharmaceutical services have remained unrecognized in mass casualty care and disaster medical services.[11] Proper incorporation of pharmaceutical services is an important element in any hospital-specific, local, and national disaster preparedness plan and represents the difference between a thriving operation and a disheveled one.[9] Pharmacists can contribute essential expertise to disaster preparedness and response, alleviating human suffering and providing appropriate pharmaceutical care.[10]
The American Society of Health-System Pharmacists has described the importance of the participation of pharmaceutical services in disaster planning and has spotlighted the top five advisory roles of health system pharmacists in disaster preparedness.[11] This ranged from advice to hospital and health-system administrators, other health-care providers, emergency preparedness planners, government agencies, state societies of health-system pharmacists, and educators respectively.[11]
In this study, we assessed the preparedness of hospital pharmacists for MCIs in Ogun State, Southwestern Nigeria. This study will form a bedrock for determining whether prevailing resources are adequate for the management of conventional MCIs as it relates to hospital pharmacists and the level of stocking of essential drugs during disasters among hospital pharmacists.
MATERIALS AND METHODS
Study location
The study was conducted in 6 major hospitals (3 tertiary health institutions: Federal Medical Centre, Idi-Aba, Abeokuta, Nigeria, Olabisi Onabanjo University Teaching Hospital, Sagamu, Nigeria, and Neuropsychiatric Hospital, Aro, Nigeria; 2 secondary health institutions: State Hospital, Ijebu-Ode, Nigeria, and State Hospital, Ijaye-Abeokuta, Nigeria, and 1 Catholic Hospital: Sacred Heart Hospital, Lantoro-Abeokuta, Nigeria.
Design
Using a 26-item structured self-administered questionnaire, a consecutive cross-sectional survey was conducted over 1 month among pharmacists working in major hospital pharmacies in Ogun State, Southwestern Nigeria.
Study population/sample size
The target population was registered pharmacists working in hospital pharmacies in Ogun State, Nigeria. Using the Raosoft Sample size calculator, an assumption of a population size of 200 hospital pharmacists with a 5% margin error and 95% confidence interval was made for a sample size of 132.
Inclusion/Exclusion criteria
The list of pharmacists used for the study was obtained from the administrative units in the government-owned tertiary and secondary health institutions and a major Catholic hospital in Ogun State, Nigeria. The pharmacists were contacted in person, and those willing to participate were included in the study. Pharmacists not working in hospitals and non-pharmacists in the pharmacy departments of the hospitals visited were excluded.
Data collection
Instrument
Data collection was through a structured self-administered questionnaire adopted from a previous study,[12] The questionnaire included 26 items: 3 items on their sociodemographic characteristics, 5 items on demographics of the hospitals where the respondents worked, 9 items on availability and preparedness for disaster plan, and 9 items on respondents’ opinions on the adequacy of medications during disaster events. The questionnaires were pre-tested among 5 pharmacists working in private hospitals before use. The responses of these pharmacists were not included in the final study data. Adjustments were made on items that were not clearly understood by the pre-testers. The purpose of the study was explained to the participants before administering the questionnaire, and difficulties with any questions were explained to the participants by one of the authors. Questionnaires were distributed by one of the researchers and filled voluntarily by pharmacists at their places of work. Participants did not to write their names on the questionnaire forms to promote anonymity.
Statistical analysis
The returned questionnaires were coded for easy reference, imputed into Microsoft Excel, double-checked to ensure the accuracy of inputted data, and exported to the Statistical Package for the Social Sciences (SPSS, version 21) for further analysis. The Chi-square was used to determine variables that had a significant association at P < 0.05. Optimal preparedness for MCIs was assumed when 50% of participants responded positively to items of preparedness on the instrument used.
Ethical approval
Ethical approval was obtained from the Federal Medical Center Abeokuta Ethics Committee. (Approval number FMCA/470/HRE/13/19). Permission was also sought and obtained from each hospital management and pharmacy. Participation in the study was fully voluntary, and there were no identifiable risks to the participants. Verbal informed consent was taken from each participant before the interview. Strict confidentiality was maintained.
RESULTS
Response rate
A response rate of 79.5% was obtained (105/132).
Sociodemographic characteristics
Forty-seven (44.8%) respondents had <10 years of working experience, 33 (31.4%) were in the age range of 26– 30 years, 62 (59.0%) were female, 63 (60.0%) were Grade1 pharmacists (the first level of pharmacist after an internship in the Nigerian hospital setting), and 82 (39.2%) respondents ran a centralized pharmacy. Further details are shown in [Table 1].
| Characteristics of respondents | Frequency (%) |
|---|---|
| Years of practice | |
| <10 | 47 (44.8) |
| 10–20 | 22 (21.0) |
| 21–30 | 18 (17.1) |
| 30 and above | 18 (17.1) |
| Age (years) | |
| <25 | 23 (21.9) |
| 26–30 | 33 (31.4) |
| 31–40 | 20 (19.1) |
| 41–50 | 17 (16.2) |
| 50 and above | 12 (11.4) |
| Gender | |
| Male | 43 (41.0) |
| Female | 62 (59.0) |
| Position held | |
| Director of pharmacy | 3 (2.8) |
| Assistant director | 7 (6.7) |
| Grade 1 Pharmacist | 63 (60.0) |
| Intern pharmacist | 22 (21.0) |
| Corper pharmacist | 6 (5.7) |
| Others (please specify) | 4 (3.8) |
| *Services of the pharmacy department | |
| Centralized pharmacy | 82 (39.2) |
| Satellite/decentralized pharmacy | 46 (22.0) |
| Unit-based pharmacist | 39 (18.6) |
| Clinical pharmacist/faculty | 40 (19.1) |
| Robotic dispensing | 2 (1.0) |
Preparedness of hospital pharmacists for MCIs
Forty-five (42.9%) respondents worked in institutions with over 400 standard beds; 66 (62.9%) pharmacists claimed that there was the availability of disaster plans. Fifty-five (55.2%) had a clear description of the pharmacy department based on the institutional protocol. [Table 2] shows further results on the availability and preparedness of the respondents for disasters.
| Variables | Frequency (%) |
|---|---|
| Does your institution have a disaster preparedness plan? | |
| Yes | 66 (62.9) |
| No | 8 (7.6) |
| Don’t know | 31 (29.5) |
| Do you have a disaster plan specifically for the pharmacy department? | |
| Yes | 48 (45.7) |
| No | 28 (26.7) |
| Don’t know | 29 (27.6) |
| How do you determine which medication to stock? | |
| Hospital committee consensus | 64 (60.9) |
| Based on other outside institutions’ policies | 9 (8.6) |
| Based on international guidelines | 3 (2.9) |
| Based on national guidelines | 19 (18.1) |
| Not applicable | 10 (9.5) |
| How are expenses for medications stock-piling covered? | |
| Federal and/or state government funding | 55 (52.4) |
| Pharmacy budget | 29 (27.6) |
| Disaster preparedness budget | 2 (1.9) |
| Not applicable | 19 (18.1) |
| Does your hospital pharmacy disaster plan include processes to ensure care is maintained for patients already in the hospital? | |
| Yes | 50 (47.6) |
| No | 4 (3.8) |
| Don’t know | 51 (48.6) |
| How often is the pharmacy involved in mock disaster preparedness | |
| Monthly | 3 (2.9) |
| Every 6 months | 3 (2.9) |
| Every 12 months | 1 (0.9) |
| Never | 20 (19.0) |
| Not applicable | 78 (74.3) |
| Based on the institutional protocol, do you feel there is a clear description of the pharmacy department? | |
| Yes | 58 (55.2) |
| No | 6 (5.7) |
| Don’t know | 41 (39.1) |
| Does your hospital pharmacy disaster plan include quantities of medications to not only treat the community but also hospital employees? | |
| Yes | 55 (52.3) |
| No | 5 (4.8) |
| Don’t know | 45 (42.9) |
Most respondents agreed that the typical disaster plan was mainly natural, 73 (35.4%); others are shown in [Figure 1]. On annual emergency department visits per year for hospitals: 37(35.2%); 30 (28.6%); and 10 (9.5%) respondents had 50,000–75,000; >75,000; and <50,000 visits, respectively. Twenty-eight (26.7%) respondents did not know how many visits they had.
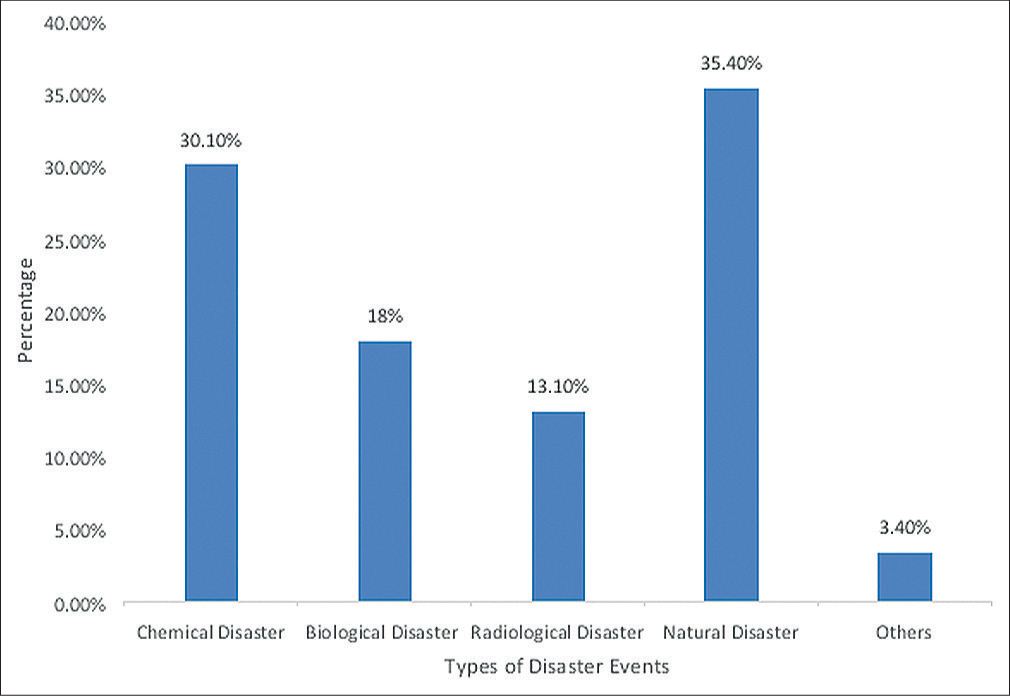
- Disaster events included in respondents’ institutional plan.
The majority of respondents, 64 (61%), strongly agreed that antiemetics should be available for disaster events. [Table 3] shows the respondents’ opinions on the availability of medications for disaster events. A Cronbach’s alpha reliability coefficient for this aspect of the survey was 0.956. There was a significant association between respondents’ year of practice and response on the inclusion of disaster events in the institutional plan (χ2 = 95.637, df = 72, and P = 0.033) on one hand, and adequacy of vasopressor/inotropic medication stocked to treat patients in the events of a disaster (χ2 = 27.556, df = 16, and P = 0.036) on the other hand. Responded positively on the adequacy of analgesics 95 (90.0%) Mean ± SD 4.42 ± 0.875 and antiemetics 89 (84.8%) Mean ± SD 4.36 ± 0.992 during disaster events.
| Types and quantities of medication needed for disaster events | SD (%) | D (%) | N (%) | A (%) | SA (%) | M (%) | ±SD |
|---|---|---|---|---|---|---|---|
| Analgesic | 3 (2.9) | 1 (1.0) | 6 (5.7) | 34 (32.4) | 61 (58.0) | 4.42 | 0.875 |
| Wound infection prophylaxis | 3 (2.9) | 3 (2.9) | 12 (11.4) | 31 (29.5) | 56 (53.3) | 4.28 | 0.976 |
| Rapid sequence intubation (sedatives and paralytics) | 1 (1.0) | 5 (4.8) | 9 (8.5) | 35 (33.3) | 55 (52.4) | 4.31 | 0.891 |
| Ophthalmic | 3 (2.9) | 5 (4.8) | 14 (13.3) | 23 (21.9) | 60 (57.1) | 4.26 | 1.047 |
| Chemical weapon antidotes | 7 (6.7) | 6 (5.7) | 12 (11.4) | 20 (19.1) | 60 (57.1) | 4.14 | 1.228 |
| Oral antimicrobials | 2 (1.9) | 2 (1.9) | 15 (14.3) | 26 (24.8) | 60 (57.1) | 4.33 | 0.927 |
| Vasopressor/inotropic | 3 (2.9) | 4 (3.8) | 13 (12.4) | 25 (23.8) | 60 (57.1) | 4.29 | 1.016 |
| Respiratory | 5 (4.8) | 5 (4.8) | 9 (8.6) | 26 (24.8) | 60 (57.1) | 4.25 | 1.108 |
| Antiemetic | 3 (2.9) | 4 (3.8) | 9 (8.6) | 25 (23.8) | 64 (61.0) | 4.36 | 0.992 |
SD: Strongly disagree, D: Disagree, N: Neutral, A: Agree, SA: Strongly agree, ±SD: Standard deviation
DISCUSSION
Disaster plans and committees are foremost in the effective management of any disaster as they establish a clear plan for how to effectively address difficulties as well as the roles and the required resource allocation during a disaster.[13]
The details of disaster planning are often lacking and not known by key stakeholders in Nigeria and other low-income nations, even though they suffer some of the deadliest disasters.[14,15]
In this study, a great number of the respondents were young both in terms of experience (nearly half have been practicing for <10 years) and age (most of the respondents are in the age range of 26–30 years [27.5%]) . It was observed that the majority of the respondents practiced in centralized settings similar to ambulatory care pharmacists. The majority of the participants were female; this corroborates with a study by Etokidem et al.,[16] where inequality in gender distribution among pharmacists in another part of Nigeria was found.[16] In many instances, and as a matter of standard procedure, disasters call for multidisciplinary collaboration among health-care workers to minimize the casualties. This is captured aptly by Descatha et al.[17] They were specifically relating emergency preparedness to workplace disasters. This multidisciplinary collaboration is also in line with the tenets of pharmaceutical care, which must be harnessed in times of disaster.[18] In terms of auxiliary infrastructure, less than half of the respondents worked in hospitals that had more than 400 standard beds. This is inadequate because infrastructure availability is an integral part of disaster preparedness. This was used to underscore surge capacity (usually underwritten by staff, space, and equipment), which measures the capacity of a facility to expand and contain a large casualty load,[19] which must be institution and preparedness specific.[9]
The majority of the respondents attested to the availability of plans for emergencies; however, 48.6 % were unaware if the hospital pharmacy disaster plan included processes to ensure care is maintained for patients already in the hospital. Typical disaster plans included those for natural, chemical, and biological disasters. For effective management of any disaster and to lay out a clear plan for how to effectively address disaster-related challenges and delineate the roles and required resource allocation, disaster plans and a disaster committee are paramount during a disaster.[20]
A significant number of the study participants agreed to the availability of sufficient quantities of medicines required in emergencies. Ongoing provision of pharmaceuticals and medical supplies are of key importance during and following a disaster or other emergency event. An effectively coordinated response involving locally available pharmacy personnel — drawing on the efforts of licensed pharmacists and support staff can help diminish harm and ease hardship in a community after emergency events.[21]
Post-event analysis of previous studies indicated that antidote stockpiling was deficient.[22] The most common justification for this perceived deficiency was the cost burden placed on hospital pharmacies in stocking rarely used pharmaceuticals.
Overall, the respondents had poor knowledge of vital disaster preparedness on issues such as the involvement of the pharmacy in mock disaster preparedness and if the hospital pharmacy disaster plan includes processes to ensure care is maintained for patients already in the hospital. Essential components of successful emergency response and integral parts of MCI preparedness and management plans should be introduced. These include adequate orientation, drills, updated training programs, conducting of simulation exercises to monitor and evaluate the emergency preparedness process of the health-care institutions, feedback on potential problems, and the development of personal and professional relationships.
There was an association between the years of practice of the pharmacists and their opinions on the adequacy of medications in disaster events. Some other researchers have also found a strong correlation between disaster preparedness and training,[23] and studies demonstrated the crucial contributions of pharmacists in hospital emergency preparedness in the United States.[24] Issues encountered during emergency situations and disasters should be included in the curricula of pharmacy schools and schools that train other health-care professionals, respectively. This would go a long way in improving knowledge and skills related to disasters.
CONCLUSION
Pharmacists have proven themselves competent in discharging their responsibilities as frontline health-care experts in the management of disasters. The results from this study show that most respondents had disaster plans in their hospitals though a third claimed ignorance on this. Over 50% of the participants admitted that there were clear descriptions of the institutional protocol for the pharmacy department and that the hospital pharmacy disaster plan includes quantities of medications to treat the community and hospital employees. They strongly agreed on the adequacy of analgesics and antiemetics in disaster events. However, preparedness for disaster preparedness was suboptimal based on the number of beds, specific disaster preparedness plan, practice for mock disasters, and lack of knowledge on basic issues of disaster planning. These results call for immediate awareness to address these shortfalls. Essential components of successful emergency response and integral parts of MCI preparedness and management plans should be introduced. These include adequate orientation, drills, updated training programs and workshops, feedback regarding potential problems, and the development of personal and professional relationships, particularly during this time of the COVID-19 pandemic.
The limitations of this study include that the study was conducted in a single city in one state of the country. Hence, results from this study may not reflect the general consensus of the pharmacy population and cannot be generalized to the entire population of pharmacists and hospitals. These respondents were majorly below 50 years of age and may have very limited experience.
Acknowledgments
We wish to appreciate all pharmacists in all the study settings who contributed toward the successful completion of this work.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
None.
References
- Mass casualty incidents-time to engage. World J Emerg Surg. 2016;11:8. doi:10.1186/s13017-016-0064-7
- [CrossRef] [PubMed] [Google Scholar]
- Defining disaster: The emergency department perspective. Proc (Bayl Univ Med Cent). 2001;14:144-149. doi:10.1080/08998280.2001.11927751
- [CrossRef] [PubMed] [Google Scholar]
- Terminology (Definition of Disaster) Available from: https://www.unisdr.org/we/inform/terminology#letter-p [Last accessed on 2021 Mar 23]
- [Google Scholar]
- 2020 U.S. Billion-Dollar Weather and Climate Disasters in Historical Context 2021. Available from: https://www.ncdc.noaa.gov>billions [Last accessed on 2021 Dec 01]
- [Google Scholar]
- WHO Declares End of Ebola Outbreak in Nigeria Statement. 2014. Available from: https://www.who.int/mediacentre/news/statements/2014/nigeria-ends-ebola/en [Last accessed on 2022 Dec 26]
- [Google Scholar]
- COVID-19 in Nigeria: A disease of hunger. Lancet Respir Med. 2020;8:556-557. doi:10.1016/S2213-2600(20)30220-4
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of knowledge, attitude and practice of disaster preparedness among Tikur Anbessa specialized hospital health care workers, Addis Ababa, Ethiopia. Am J Nurs Sci. 2018;7:39-48. doi:10.11648/j.ajns.20180701.15
- [CrossRef] [Google Scholar]
- Disaster and mass casualty management in a hospital: How well are we prepared? J Postgrad Med. 2006;52:89-90.
- [Google Scholar]
- Hospital disaster preparedness in the United States: New issues, new challenges. IJRDM. 2004;4
- [CrossRef] [Google Scholar]
- Medical Surge Capacity: Workshop Summary; Forum on Medical and Public Health Preparedness for Catastrophic Events United States: National Academies Press; 2010.
- [Google Scholar]
- ASHP statement on the role of health-system pharmacists in emergency preparedness. Am J Health Syst Pharm. 2003;60:1993-1995. doi:10.1093/ajhp/60.19.1993
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of hospital pharmacy preparedness for mass casualty events. P T. 2015;40:264-267.
- [Google Scholar]
- Disaster metrics: Quantitative benchmarking of hospital surge capacity in trauma-related multiple casualty events. Disaster Med Public Health Prep. 2011;5:117-124. doi:10.1001/dmp.2010.19
- [CrossRef] [PubMed] [Google Scholar]
- Effect of hospital staff surge capacity on preparedness for a conventional mass casualty event. West J Emerg Med. 2010;11:189-196.
- [Google Scholar]
- Disaster preparedness of Canadian trauma centres: The perspective of medical directors of trauma. Can J Surg. 2011;54:9-16. doi:10.1503/cjs.022909
- [CrossRef] [PubMed] [Google Scholar]
- Influenza A H1NI (Pandemic 2009): How prepared are healthcare providers in Calabar, Nigeria? J Infect Dis Immun. 2012;4:23-28.
- [CrossRef] [Google Scholar]
- Emergency preparedness and response in occupational setting: A position statement. Front Public Health. 2017;5:251. doi:10.3389/fpubh.2017.00251
- [CrossRef] [PubMed] [Google Scholar]
- Pharmaceutical care: Past, present and future. Curr Pharm Des. 2004;10:3931-3946. doi:10.2174/1381612043382521
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation and analysis of hospital disaster preparedness in Jeddah. Health. 2014;6:2668-2687. doi:10.4236/health.2014.619306
- [CrossRef] [Google Scholar]
- Mass casualty incidents and disasters in Nigeria: The need for better management strategies. Niger Postgrad Med J. 2007;14:341-346.
- [CrossRef] [PubMed] [Google Scholar]
- Defining roles for pharmacy personnel in disaster response and emergency preparedness. Disaster Med Public Health Prep. 2017;11:496-504. doi:10.1017/dmp.2016.172
- [CrossRef] [PubMed] [Google Scholar]
- Atropine availability as an antidote for nerve agent casualties: Validated rapid reformulation of high-concentration atropine from bulk powder. Ann Emerg Med. 2003;41:453-456. doi:10.1067/mem.2003.103
- [CrossRef] [PubMed] [Google Scholar]
- Emergency and disaster management training; knowledge and attitude of Yemeni health professionals-a cross-sectional study. BMC Emerg Med. 2018;18:23. doi:10.1186/s12873-018-0174-5
- [CrossRef] [PubMed] [Google Scholar]
- Hospital emergency preparedness: Push-POD operation and pharmacists as immunizers. J Am Pharm Assoc (2003). 2012;52:81-85. doi:10.1331/JAPhA.2012.11191
- [CrossRef] [PubMed] [Google Scholar]







