Translate this page into:
Primary pyogenic ventriculitis caused by Streptococcus intermedius
Corresponding author: Timothy Daly, DO, MS St. Luke’s University Hospital, 801 Ostrum Street, Bethlehem, PA 18015, Pennsylvania, United States. Timothy.daly@sluhn.org
-
Received: ,
Accepted: ,
How to cite this article: Daly T, Ramos-Feliciano K, Titus M, et al. Primary pyogenic ventriculitis caused by Streptococcus intermedius. Am J Pharmacother Pharm Sci 2022;10.
Abstract
Pyogenic ventriculitis is a rare infection especially when it occurs without any prior central nervous system instrumentation. We present a case of severe Streptococcus intermedius ventriculitis in an immunocompetent host.
Keywords
Ventriculitis
Streptococcus intermedius
Antibiotics
Pyogenic
Central nervous system
INTRODUCTION
Streptococcus intermedius is a β-hemolytic, Gram-positive bacterium that belongs to the Streptococcus anginosus group, formerly known as Streptococcus milleri.[1] Members of this group include S. intermedius, S. anginosus, and Streptococcus constellatus, all of which are commensal organisms found in the normal flora of the oral cavity, genitourinary tract, and gastrointestinal tract.[2] These organisms are unique for their propensity to cause abscess formation and are less commonly associated with endocarditis than viridian streptococci.[3] Nearly, all isolates of S. intermedius, most isolates of S. constellatus, but only 19% of those of S. anginosus, were associated with abscess.[4] S. intermedius is believed to be clinically associated with brain and liver abscess;[2] however, reported cases of S. intermedius linked to meningitis remain relatively low.
Here, we present a rare case of severe ventriculitis caused by S. intermedius.
CASE REPORT
The patient was a 62-year-old male with a medical history of hypertension, hyperlipidemia, previous ischemic stroke on aspirin daily, and obstructive sleep apnea that presented to an outside hospital with persistent nausea, vomiting, and diarrhea. The patient ate seafood 3 days prior and reported vomiting shortly after. The family was initially concerned about food poisoning. The patient had progressive vomiting, malaise, and lightheadedness through the weekend. On the day of admission, the patient also complained of headaches. He was admitted to the medical floor as a case of viral gastroenteritis. His clinical condition worsened with acute onset disorientation, confusion, and eye rolling necessitating a stroke alert and further brain imaging including a computed tomography/computed tomography angiogram of the head and, subsequently, a magnetic resonance imaging (MRI) of brain. Endotracheal intubation and mechanical ventilation were needed for airway protection.
MRI of the brain was consistent with ventriculitis, with debris in the ventricles and possible developing abscess as seen in Figure 1. The patient was started on vancomycin, ceftriaxone, and ampicillin. He underwent an external ventricular drain placement with elevated opening pressure and significant CSF pleocytosis. CSF sampling also revealed a protein of 1103 mg/dL, glucose of 6 mg/dL, and more than 250,000 white blood cells. Multiple CSF cultures grew S. intermedius. Antibiotic therapy was deescalated to high-dose ceftriaxone and with persistent fever, a short course of four doses of intrathecal vancomycin was also administered.
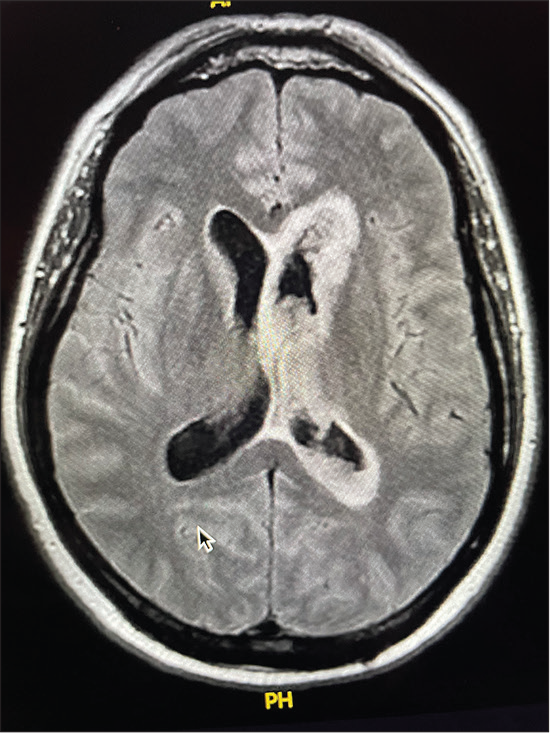
- MRI showing diffuse ependymal enhancement not throughout the ventricular system with debris present, most consistent with ventriculitis.
CT of the face showed bilateral mastoid effusions and right serous otitis, but no dental abscess. Transthoracic echocardiogram was performed to rule out endocarditis and showed no vegetations. CT of the abdomen and pelvis showed no intra-abdominal source of infection. The patient’s last colonoscopy was 2 years prior without concerning findings. A myringotomy and tube tympanostomy in the right ear on by otolaryngology showed no evidence of infected fluid. A repeat MRI brain 2 weeks after admission showed persistent ependymal enhancement and hydrocephalus.
Persistent fever and concerns for drug fever necessitated antibiotic switch to high-dose ampicillin which was continued for a total 6-week course. With persistent hydrocephalus, a ventriculoperitoneal (VP) shunt was inserted after resolution of fevers and sterility of cerebrospinal fluid. This was complicated by VP shunt malfunction initially requiring externalization of shunt and subsequently re-insertion of VP shunt.
After a prolonged hospital stay of 51 days, he was eventually discharged to a rehabilitation facility.
DISCUSSION
S. intermedius is present in oral, genitourinary, and gastrointestinal cavities as commensal organism and can be a cause for brain abscesses in immunocompromised individuals. Patients with CSF or blood cultures positive for this organism should be worked up for causes, leading to hematogenous spread from a distant focus.[5,6]
This organism has distinctive features including a subacute presentation, lack of bacteremia, and a prolong course of infection when compared with S. pneumonia. These characteristics, combined with the development of brain abscesses, should raise suspicion for a CNS infection caused by S. intermedius or other S. milleri group species.[5,6] In our patient’s brain MRI, debris in the ventricles and a possible abscess was observed. These findings, along with patient’s presentation, match with this bacterium’s rare presentation.
A few cases of meningitis/pyogenic ventriculitis caused by S. intermedius have been reported in the medical literature. Although the exact mechanism remains unknown; polysaccharide capsules, pyrogenic exotoxins, and hydrolytic enzymes are thought to play an important role as virulence factors leading to abscess formation. Furthermore, this organism mostly affects patients with underlying conditions, including those immunocompromised.[6-8]
CNS infections including brain abscesses known to be caused by S. intermedius species may be treated with intravenous ceftriaxone therapy, and the treatment should be continued for 4–6 weeks. If there are concerns for a b-lactam allergy, clindamycin and vancomycin can be used as its penicillin resistance is <2%.[9]
Obstructive hydrocephalus is a common complication of ventriculitis due to ependymal lining inflammation, leading to the impairment of the CSF flow in the brain. Two cases of meningoventriculitis caused by S. intermedius leading to adhesions and multiloculated hydrocephalus have been reported, associated with a decompensation including respiratory failure and seizures and the requirement of a ventriculostomy for decompression.[10,11] It is not a common complication of this organism, as it is mostly associated with abscesses rather than meningitis or ventriculitis, but, when present, it can be fatal. As in our patient, in those cases, numerous surgical interventions were needed to control them and no predisposing factors or source of infection were identified.
Although S. intermedius is a rare cause of meningitis, subacute presentation, and presence of suppurative infections should raise suspicion for its etiology.[3] Our patient represents an unusual case of ventriculitis caused by S. intermedius, an uncommon bug with characteristic features.
CONCLUSION
This patient presents a rare, severe ventriculitis caused by S. intermedius. He had no prior CNS instrumentation and no obvious source of a bacterial meningeal infection.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
References
- From normal flora to brain abscesses: A review of Streptococcus intermedius. Front Microbiol. 2020;11:826.
- [CrossRef] [PubMed] [Google Scholar]
- Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (the Streptococcus milleri group): Association with different body sites and clinical infections. J Clin Microbiol. 1992;30:243-244.
- [CrossRef] [PubMed] [Google Scholar]
- Streptococcus intermedius causing infective endocarditis and abscesses: A report of three cases and review of the literature. BMC Infect Dis. 2008;8:154.
- [CrossRef] [PubMed] [Google Scholar]
- Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus ("Streptococcus milleri group") are of different clinical importance and are not equally associated with abscess. Clin Infect Dis. 2001;32:1511-1515.
- [CrossRef] [PubMed] [Google Scholar]
- Streptococcus intermedius: A cause of lobar pneumonia with meningitis and brain abscesses. Clin Infect Dis. 2000;30:396-397.
- [CrossRef] [PubMed] [Google Scholar]
- Streptococcus milleri pulmonary disease: A review and clinical description of 25 patients. Thorax. 1995;50:1093-1096.
- [CrossRef] [PubMed] [Google Scholar]
- Culture-negative intracerebral abscesses in children and adolescents from Streptococcus anginosus group infection: A case series. Clin Infect Dis. 2008;46:1578-1580.
- [CrossRef] [PubMed] [Google Scholar]
- Meningitis and brain abscess caused by Streptococcus intermedius in a patient infected with HIV-1. An Med Interna. 2005;22:279-282.
- [CrossRef] [Google Scholar]
- Antibiotic susceptibilities of genetically characterized Streptococcus milleri group strains. Antimicrob Agents Chemother. 2001;45:1511-1514.
- [CrossRef] [PubMed] [Google Scholar]
- A Streptococcus intermedius brain abscess causing obstructive hydrocephalus and meningoventriculitis in an adult patient with chronic granulomatous disease. Can J Gen Intern Med. 2015;10:2.
- [CrossRef] [Google Scholar]
- Primary ventriculitis caused by Streptococcus intermedius. Br J Neurosurg. 2007;21:293-296.
- [CrossRef] [PubMed] [Google Scholar]






