Translate this page into:
Relative bioavailability study of ticagrelor in healthy subjects under fasting conditions
*Corresponding author: Evelyn Pena, MSc. MD. Department of Clinical Research, Industrias Biocontrolled C.A., Laboratorios Leti S.A.V., Guarenas, Miranda, Venezuela. martinpena24@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pena E, Inatti A, Taly A, et al. Relative bioavailability study of ticagrelor in healthy subjects under fasting conditions. Am J Pharmacother Pharm Sci 2024:8.
Abstract
Objectives:
This is a randomized, single-dose, two-period, two-sequence, and crossover study to evaluate the bioequivalence (BE) profiles of two formulations of ticagrelor 90 mg, under fasting conditions.
Materials and Methods:
The plasma concentrations of ticagrelor were measured using a validated liquid chromatography mass spectrometry method. Enrolled for the study were 30 healthy adult volunteers (21 males and 9 females). All completed the study. The two formulations of ticagrelor were considered bioequivalent if a 90% confidence interval (CI) fell within 80.00–125.00% for Cmax and AUC0-t. Tolerability and safety were assessed throughout the study.
Results:
The pharmacokinetic (PK) parameters were similar between the test product (T) Clenosan® and reference product (R) Brilinta® under fasting conditions (90% CI for all PK parameters fell within 80.00–125.00%). The 90% CI of the test/reference ratios of log-transformed PK parameter point estimates were Cmax: 95.49% (87.99– 103.62%) and AUC0-t: 103.20% (97.52–109.21%), respectively.
Conclusion:
Our results demonstrated BE between the test and reference drug products of oral ticagrelor in healthy subjects under fasting conditions.
Keywords
Bioequivalence
Ticagrelor
Healthy subject
Single dose
Pharmacokinetic
INTRODUCTION
Ticagrelor is a potent oral platelet P2Y12 receptor antagonist that directly inhibits a central amplification pathway of platelet activation.[1] Ticagrelor was approved (2010) for the prevention of atherothrombotic events in patients with acute coronary syndrome (ACS).[2] Ticagrelor coadministered with low dose of acetylsalicylic acid is indicated for secondary prevention of atherothrombotic events in patients with ACS and a history of myocardial infarction (MI). Ticagrelor is also indicated to reduce the risk of first MI or stroke in patients with coronary artery disease, type 2 diabetes, and a history of percutaneous coronary intervention, who are at high risk of developing an atherothrombotic event.[2-4]
Ticagrelor achieves rapid absorption from the gastrointestinal tract and a rapid onset of action with an average oral bioavailability of approximately 36% (range 25.4–64%) due to hepatic first-pass metabolism.[1,5,6] There are ten metabolites, the predominant active metabolite is ARC124910XX, a product of the cytochrome P450 (CYP)3A4/5 enzymes.[1,5,6] Both ticagrelor and its active metabolites are highly bound to plasma proteins (>99.7%).[1,6] Ticagrelor and its mean metabolite reach a maximum plasma concentration (Cmax) after about 1.5 and 2.5 h, respectively.[1,5,6] The Cmax and AUC increased proportionally with dose over the dose range studied (30–1260mg).[5,6] Based on a population PK analysis of the PEGASUS study, the median ticagrelor Cmax was 391 ng/mL and AUC was 3801 ng*h/mL at steady state.[6] The steady-state volume of distribution of ticagrelor is 87.5L.[5,6] The primary route of ticagrelor elimination is via hepatic metabolism and the active metabolite is likely through biliary secretion.[6] The mean T1/2 was approximately 6.9 h (range 4.5–12.8 h) for ticagrelor and 8.6 h (range 6.5–12.8 h) for the active metabolite.[5,6] The PK profile of ticagrelor is not significantly affected by age, gender, or administration with food.[5,6]
Ticagrelor was approved by the European Medicines Agency (EMA) and The United States Food and Drug Administration (FDA) in 2010 and 2011, respectively.[1,6,] The current US FDA recommendations for dosing and administration of ticagrelor include an oral loading dose of 180 mg followed by 90 mg twice daily (Brilinta®, prescribing information).[1,6-8]
The purpose of our study was to assess and compare the PK profiles and safety of Brilinta® (AstraZeneca AB, Sweden) as reference (R) formulation to Clenosan® (Laboratorios Leti, S.A.V., República Bolivariana de Venezuela) as test (T) formulation of ticagrelor 90 mg, in healthy adult subjects in randomized crossover study.
This study was conducted by a clinical research operator VerGo Pharma Research Pvt. Ltd., India.
MATERIALS AND METHODS
Ethical approval
The study was conducted ethically in accordance with the principles of the ICMR guidelines (2017),[9] New Drugs and Clinical Trials Rules 2019 India,[10] and adhered to the ethical principles of the Declaration of Helsinki,[11] the International Conference on Harmonization Good Clinical Practice Guidelines.[12] The study protocol (N°022-23) was approved by Aavishkar Ethical Committee, on June 24, 2023 (Version:00, Dated May 29, 2023) and certified by CDSCO/DGHS to VerGo Clinical Research Pvt, Ltd.
Study design
This was a randomized, single oral dose, two-treatment, two-period, two-sequence, and crossover bioequivalence (BE) study under fasting conditions comparing two ticagrelor formulations. Clenosan® 90 mg coated tablets were provided as the test formulation (T) by Laboratorios Leti S.A.V, República Bolivariana de Venezuela, batch N°002, date of expiry 08/2024, and the reference formulation (R) Brilinta® 90 mg coated tablets by AstraZeneca AB, Sweden, batch N°56943, date of expiry 03/2024.
The subjects were randomized, to one of the two sequences (T R) or (R T). The randomization schedule was generated using Statistical Analysis Software (SAS® version 9.4). One single dose was administered in each period. Subjects who received T product in period I were administered R product in period II and vice versa. The pre-screening period was 21 days. The study lasted for 10 days (August 18–27, 2023) with 7 days washout period, considering the terminal half-life for ticagrelor is 12.8 h.[5,6]
Subjects
All volunteers underwent a screening procedure. Thirty healthy volunteers (21 males and 9 females) who met the inclusion and exclusion criteria were enrolled. They had a mean age of 34.0 years, mean weight of 66.64 kg, mean height of 162 cm, and body mass index of 25.04 kg/m2 [Table 1].
| Age | Mean±SD | 34±6.45 | ||||
| (years) | Range | 20–43 | ||||
| Age group | F | % | M | % | Total | |
| 18–40 | 6 | 20 | 17 | 56.65 | 23/76.65 | |
| 41–64 | 3 | 10 | 4 | 13.35 | 7/23.35 | |
| Total | 20–43 | 9 | 30 | 21 | 70 | 100 |
| BMI (kg/m2) | Mean±SD | 24.57±2.7 | ||||
| Range | (18.59–29.74) | |||||
| Race | Asian | 30 | 100 | |||
BMI: Body mass index, SD: Standard deviation
A complete clinical history valid for 6 months before the start of the study; normal laboratory values as determined by medical history and physical examination at the time of screening; normal vital signs and physical examination; creatinine clearance of more than 50 mL/min; negative tests for hepatic transaminases, hepatitis B and C, human immunodeficiency virus, and venereal diseases research laboratory; and normal 12-lead EKG values, normal chest radiography, and negative result in urine drug tests. Serum pregnancy test for female volunteers during screening and urine pregnancy test, urine for drugs of abuse, and urine test for alcohol consumption were performed on the day of check-in of each period. Activated partial thromboplastin time (aPTT) and partial thromboplastin international normalized ratio (PT-INR) tests were performed before the check-in of period I. Another key inclusion criterion was that subjects must be non-smokers or smokers who had not smoked at least 10 h before the start of the study. They all signed the informed consent.
The exclusion criteria included volunteers incapable of understanding the informed consent, a history of diabetes, tuberculosis, and systemic hypertension. A history of hypersensitivity to the study medication or any other medication belonging to the study group or cardiovascular, renal, hepatic, metabolic, gastrointestinal, neurological, endocrine, hematopoietic, psychiatric, or other organic abnormalities; under medication that interferes with the quantification, drugs that can potentially affect the hepatic metabolism of other drugs.
Drug administration
The subjects were admitted to the facility overnight before the study. In each period, after overnight fasting of 10 h, each subject received a single oral dose (1 × 90 mg) of either one T or R, following a randomization schedule with 240 mL ± 2 mL of water at ambient temperature in a sitting position for 2 h after dosing. A total of 23 × 6 mL of venous blood samples were collected through cannula from each subject during each period, withdrawn at pre-dose (00-00 h) and 00.33, 00.67, 01.00, 01.33, 01.67, 02.00, 02.33, 02.67, 03.00, 03.50, 04.00, 04.50, 05.00, 05.50, 06.00, 08.00, 10.00, 12.00, and 16.00 h. While 24.00, 34.00, and 48.00 h, post-dose, blood samples were collected by direct venipuncture. The subjects received standardized meals (2500 Kcal) and drinking water was provided ad libitum.
Analytical procedure
Venous blood samples were collected in pre-labeled K2EDTA (ethylenediaminetetraacetic acid) vacutainers and were centrifuged at 3800 rpm for 10 min at 10°C within 45 min of sample collection. Plasma was separated, labeled, and stored at –70°C ± 15 °C before analysis. Subsequently, the plasma samples were processed, a calibration curve of internal standards (IS) Ticagrelor D7, (Vivian Life Sciences Private Limited, Mumbai, India), and quality control (QC) samples were thawed and vortexed for preparation and analysis. Ticagrelor was selectively isolated from 200 μL plasma by liquid–liquid extraction method. Aliquots of 200 μL plasma were mixed with 50 μL of ISTD working dilution and 50 μL of 5% formic acid solution and vortexed, then 2 mL of methyl tertiary butyl ether was added and vortexed for 10 min. All samples were centrifuged for 10 min at 10.0°C ± 2.0 at 4000 rpm. The supernatant was separated from the organic layer and transferred to another set of pre-labeled tubes. The samples were dried using a nitrogen evaporator at 4.0°C ± 2.0 for 10 min. The samples were reconstituted with 300 μL of mobile phase and vortexed. The tubes were transferred to pre-labeled autosampler vials. Control samples were spiked with internal standard (IS) over the concentration range of 5.009–1501.800 ng/mL. Samples of plasma, IS, and quality control (QC) were transferred to pre-labeled vials arranged into the autosampler at 10°C ± 2°C and injected in a liquid chromatography electrospray ionization tandem mass spectrometry instrument (LCESI-MS-MS) (Shimadzu BA LCMS/099, Mumbai, India). The chromatographic separation was performed by ACE 5 C18 100 × 4.6 mm high-performance liquid chromatography (HPLC) column (Shimadzu). The injection volume was 10 μL (Autosampler SIL-30ACMP, pump: LC-30AD, column oven CTO-20A) with a mobile phase of organic mixture: 020%, formic acid solution: 60/40 vv with a time retention to ticagrelor of 5.05 min (±0.50) and ISTD: 4.96 min (±0.50). The mass spectrometer was operated in positive electrospray mode. Identifications were based on multiple reactions monitoring transitions; m/z 523.10–153.10 for ticagrelor and m/z 530.00–153.10 for the IS-Ticagrelor D7. The inter-batch calibration standard was 2.43–3.13% with an accuracy 103.00–98.00%.
Statistical analysis
The sample size calculation for the study was based on the intra-subject coefficient of variation (CV%) for ticagrelor obtained from published literature (Cmax:17%, and AUC0-t 28%), with the expected % CV not exceeding 20% and the ratio within 80% and 125%.[6,13,14] The study required 28 evaluable subjects to demonstrate BE with a power of ≥80% at a 5% level of significance. Based on a sample size, 30 subjects were sufficient to demonstrate BE between the two ticagrelor formulations. Statistical analysis was conducted on all of the subjects, who completed both periods of the study as per protocol, using SAS® (software version 9.4, Institute. Inc., CARY, USA).
The primary PK parameters were evaluated and adhered to EMA-Specific Ticagrelor BE Guide,[15] maximum peak concentration (Cmax) and area under curve from time 0 to last measurable concentration (AUC0-t). Other PK parameters evaluated were as follows: Time to reach Cmax (Tmax), the time required for the plasma concentration to decrease by 50% (T1/2), area under the plasma concentration–time curve from time 0 to infinity (AUC0-inf), AUC_% Extrap, constant of elimination (Kel), and the number of points (Npoints) of the terminal log-linear phase used to estimate the terminal rate constant. The natural log-transformed (i.e., Ln-transformed) values for PK parameters Cmax and AUC0-t were analyzed for statistical difference between test and reference formulations with analysis of variance (ANOVA) by a Generalized Linear Model ANOVA using SAS®. Based on these parameters, the 90% confidence intervals (CIs) were constructed for the least square mean differences of log-transformed PK parameters Cmax and AUC0-t for ticagrelor. The formulations were regarded as bioequivalent when the 90% CIs of the T and R ratio of Cmax and AUC0-t, ranged from 80% to 125%. This is the BE standard accepted by EMA.[15,16]
Safety assessments
The safety of two formulations was evaluated through the assessment of adverse events (AEs) monitoring throughout the study. Vital signs were measured during baseline screening and at the conclusion of the study. Twelve-lead electrocardiogram and clinical laboratory including aPTT and PT-INR tests were performed before the study check-in, and the hematology evaluation was carried out 48 h post study.
RESULTS
All subjects (30) completed the study and were included in the PK and statistics evaluation. A non-compartmental analysis was applied for the estimation of PK parameters Cmax, AUC0-t, Tmax, Kel (h−1), and T½, of ticagrelor in plasma concentration which are presented in Tables 2 and 3, analysis of variance analysis from Ln Cmax, and LnAUC0-t. The oral dosing of ticagrelor 90 mg for 48 h post-dose is represented on arithmetic and logarithmic scales as shown in Figures 1 and 2. The test/reference geometric mean ratios and 90% CIs for the logarithm of Cmax and AUC0-t are presented in Table 3. The BE results were as follows: Ln Cmax 95.49% (87.99–103.62%) and AUC0-t: 103.20% (97.52–109.21%); these values are within the 90% CIs and acceptance criteria of 80–125% [Table 3]. There were no significant differences between the PK parameters of the two ticagrelor formulations (P > 0.05). These results met the predefined BE requirements.[15]
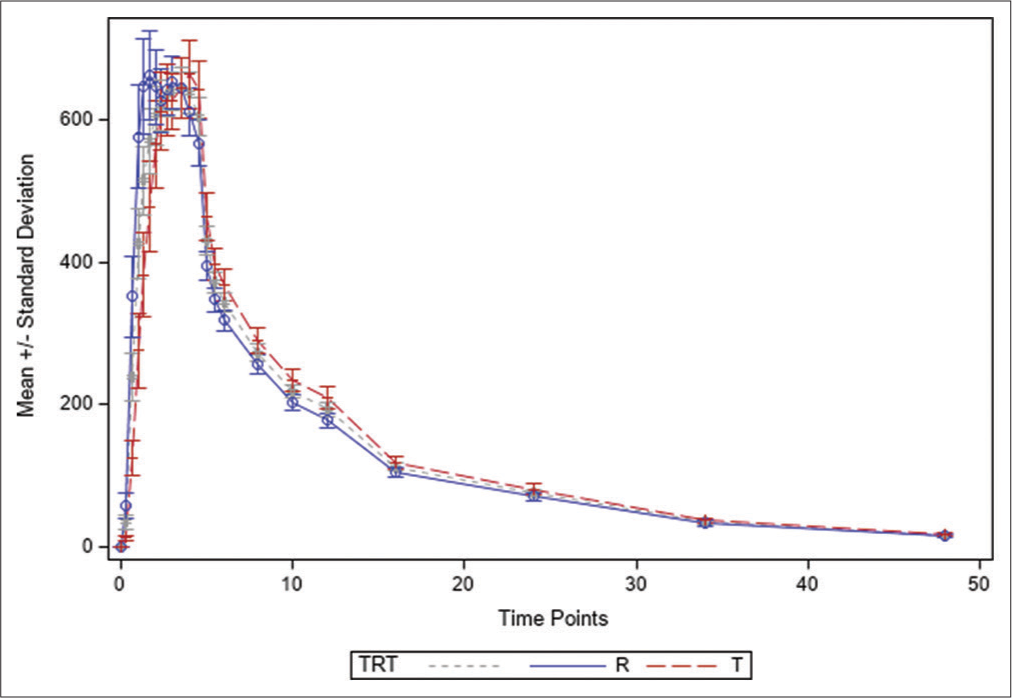
- Ticagrelor plasma concentration vs time profile for each formulation, test (T) and reference (R). Arithmetic scale.
| Time (h) | Mean Ticagrelor 90 mg data Reference (R) µ/mL |
SD Data Reference (R) |
Geometric Mean Ticagrelor Reference (R) |
Mean Ticagrelor 90 mg data Test (T) µ/mL | SD Data Test (T) |
Geometric Mean Ticagrelor Test (T) |
|---|---|---|---|---|---|---|
| 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 0.33 | 57.68 | 99.31 | 0.00 | 12.76 | 21.55 | 0.00 |
| 0.67 | 352.71 | 311.48 | 196.05 | 125.50 | 130.78 | 0.00 |
| 1.00 | 576.04 | 395.55 | 421.35 | 276.71 | 287.30 | 144.70 |
| 1.33 | 647.07 | 370.16 | 520.93 | 382.64 | 328.09 | 246.35 |
| 1.67 | 662.72 | 343.22 | 561.47 | 478.60 | 349.98 | 347.06 |
| 2.00 | 646.06 | 291.00 | 573.88 | 565.83 | 335.43 | 449.75 |
| 2.33 | 627.45 | 245.56 | 580.64 | 612.35 | 303.76 | 520.95 |
| 2.67 | 643.24 | 197.10 | 617.25 | 627.88 | 278.89 | 555.36 |
| 3.00 | 652.94 | 201.31 | 625.51 | 626.34 | 215.23 | 583.14 |
| 3.50 | 644.83 | 227.35 | 608.93 | 643.88 | 231.73 | 600.02 |
| 4.00 | 311.25 | 186.75 | 584.59 | 663.89 | 263.13 | 618.85 |
| 4.50 | 567.36 | 176.50 | 540.52 | 641.69 | 219.10 | 604.73 |
| 5.00 | 395.41 | 108.93 | 380.09 | 464.78 | 183.77 | 432.45 |
| 5.50 | 347.67 | 91.42 | 334.58 | 396.77 | 124.17 | 376.45 |
| 6.00 | 318.34 | 84.45 | 306.71 | 368.63 | 120.29 | 348.29 |
| 8.00 | 256.30 | 72.25 | 245.39 | 290.72 | 100.04 | 273.23 |
| 10.00 | 203.46 | 58.22 | 194.48 | 235.00 | 84.39 | 220.59 |
| 12.00 | 178.10 | 58.21 | 169.68 | 209.29 | 85.24 | 194.62 |
| 16.00 | 105.70 | 38.82 | 98.73 | 119.43 | 48.91 | 110.69 |
| 24.00 | 70.81 | 33.59 | 64.93 | 81.68 | 43.36 | 73.32 |
| 34.00 | 33.31 | 22.78 | 2825 | 37.43 | 21.75 | 32.52 |
| 48.00 | 16.04 | 14.28 | 0.00 | 17.60 | 11.95 | 14.59 |
SD: Standard deviation
| PK Parameters (Units) |
Ticagrelor 90 mg | |
|---|---|---|
| Clenosan® (T) | Brilinta® (R) | |
| Cmax(ng/mL) | 827.90±280.62 | 860.62±272.49 |
| AUC0-t(h*ng/mL) | 6859.01±2146.69 | 6592.26±2066.39 |
| Tmax (h) | 2.92±1.05 | 2.21±0.98 |
| T1/2 (h) | 10.39±1.66 | 10.39±2.47 |
| Kel (1/h) | 0.068±0.010 | 0.069±0.011 |
Data presented as a mean±standard error. Cmax: Maximum concentration, AUC0-t: Area under the plasma concentration–time curve from time 0 to the last measurable concentration, Kel: Elimination rate constant, Tmax: Time to reach Cmax, T1/2: Time required for plasma concentration to decrease by 50%, PK: Pharmacokinetic
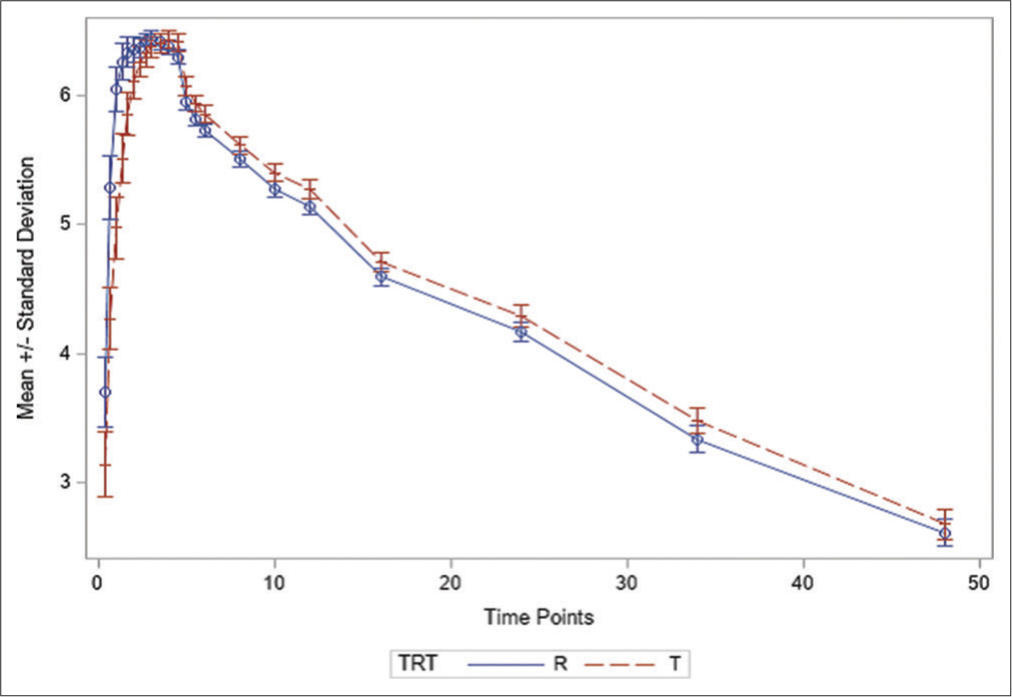
- Ticagrelor plasma concentration vs time profile for each formulation, test (T) and reference (R). Logarithmic scale.
DISCUSSION
The present study was designed to evaluate the BE in one single-dose study of two treatments, two periods, and crossover n healthy subjects volunteers of both sexes under fasting conditions under the EMA guidelines.[15] The 90% CIs for ticagrelor was assessed determined BE standards of 80–125% for Cmax and AUC0-t.[15-17] The study included 30 subjects (nine females and 21 males) covering the variability observed in other studies with a sufficient number of subjects to ensure statistical power to demonstrate the BE of both formulations.[13,16]
The PK mean values of Cmax and AUC0-t were 783.69 ng/mL and 6531.06 h*ng/mL to T and 820.74 ng/mL and 6328.60 h*ng/mL to R formulations, respectively, which included into the range of BE acceptance limit of 80–125% [Table 3].[14-16] Other parameters evaluated were T½ (10.39 ±1.66 h and 10.39±2.47 h) for the T product and R product, respectively [Table 3].
The 90% CIs for GMRs ranged from Ln Cmax was 95.49% with CIs (87.99–103.62) and AUC0-t was 103.20% with CIs (97.52–109.21) [Table 4].
| Parameters (units) | Geometric mean ratio GMR | Ratio (%) (T/R) | 90% CIs (%) | Power (T vs. R) (%) | |
|---|---|---|---|---|---|
| T | R | ||||
| Ln (Cmax) (ng/mL) |
783.69 | 820.74 | 95.49 | 87.99 – 103.62 | 99.67 |
| Ln (AUC0-t) (h *ng/mL) |
6531.06 | 6328.60 | 103.20 | 97.52 – 109.21 | 100.0 |
Data presented as a % mean Ln transformed. Cmax: maximum concentration, AUC0-t: area under the plasma concentration–time curve from time 0 to the last measurable concentration, BE acceptance criteria of 80–125%, GMR: geometric mean ratios, CI: confidence interval, PK: pharmacokinetic.
The mean ticagrelor plasma concentrations-time curves of T product versus R product, in arithmetic and logarithmic scale, were similar [Figures 1 and 2]. BE was demonstrated between the T product Clenosan® and R product Brilinta®, oral tablets at a dose of 90 mg, in fasting condition. Ticagrelor has been recommended by the American College of Cardiology Foundation in the management of atherothrombotic events in primary and secondary prevention. Ticagrelor is also recommended in patients at high risk of cardiovascular events; diabetics type 2 and patients with kidney dysfunction.[1-4,6,8]
Regulatory agencies in Latin America are demanding more attention in the process of conducting BE studies to make decisions ensuring greater access and adherence to these treatments, especially in chronic diseases.[17-19] This study will be of great support to introduce new generic drugs in Latin American countries.
Tolerability and safety
The study safety was evaluated using AEs and laboratory test. A total of 01 AEs was reported in this study, during in-house stay, and 02 AEs were reported during post study laboratory safety assessment. The incidence of AEs for each treatment is reported in Table 5.
|
Category Clinical/Laboratory |
Test n=30 AEs: 02/6.66 |
Reference n=30 AEs: 01/3.33 |
Safety Correlation with treatment (yes or not ) |
Clinically S NS |
||
| CNS (01) (Subject N°27) Dizziness |
3.33 | - | NR | NS | ||
|
Hematology AEs Lab (02) |
Screening Sample Value (%) |
Post study Sample Value (%) |
Screening Sample Value (%) |
Post study Sample Value (%) |
Normal ranges safety correlation |
S or NS |
| Increased Eosinophils (Subject N°04) |
35.6% (3.33) |
55% | - | - | (5–50%) | S |
| Increased Lymphocytes (Subject N°13) |
4.6% (3.33) |
12% | (0.9%) | S | ||
Adverse events (AEs) are presented by category in clinical and laboratory in the two treatments (test and reference). BE: Bioequivalence. AEs: Adverse events. Safety correlation: Significance (S) or No significance (NS). AEs Lab: Laboratory adverse events. NR: Not related. CNS: Central nervous system.
No severe or serious AEs were reported during the course of the study.
All the AEs were resolved completely without any sequelae. There was no death reported during the course of the study. Hence, the T and R formulations were found to be safe and well tolerated.
Limitations of the study
We did not evaluate the PK of the major active metabolite AR-C124910XX for supportive evidence of BE. In the study, we did not analyze PK data for truncated AUC (AUC 0–72 h) as recommended by EMA guidance for the drug product. An acceptable fasting BE study alone does not meet the requirements for approval of ticagrelor tablets under the guidelines of other regulatory agencies. According to US FDA guidelines, two-treatment, and two-period crossover BE studies under fasting and fed conditions are required to assess BE.[20]
CONCLUSION
This study of a single oral dose of ticagrelor 90 mg demonstrated BE of the T product, Clenosan® to R product, and Brilinta®, in healthy subjects under fasting conditions. The PK profiles for both ticagrelor products were similar and demonstrated by the 90% CIs of Cmax and AUC0-t within the accepted BE criteria of 80–125%.
Acknowledgments
This study was conducted at the third party Pharmadesk Solutions Pvt., Ltd., and VerGo Pharma Research Pvt. Ltd, (Division-VerGo Clinicals). India.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The author certifies that they have obtained all appropriate patient consent.
Conflicts of interest
All authors are Industrias Biocontrolled C.A. (A Leti Group company) employees and may hold share and/or stock options in the company . The authors have no other potential conflicts of interest relevant to this study.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
This study was funded by Laboratorios Leti, S.A.V.
References
- Ticagrelor: Clinical development and future potential. Rev Cardiovasc Med. 2021;22:373-394. doi: 10.31083/j.rcm2202044
- [CrossRef] [PubMed] [Google Scholar]
- Ticagrelor: A review of its use in the management of acute coronary syndromes. Drugs. 2011;71:909-933. doi: 10.2165/11206850-000000000-00000
- [CrossRef] [PubMed] [Google Scholar]
- Oral antiplatelet therapy after acute coronary syndrome: A review. JAMA. 2021;325:1545-1555. doi: 10.1001/jama.2021.0716
- [CrossRef] [PubMed] [Google Scholar]
- Comparative effects of guided vs. potent P2Y12 inhibitor therapy in acute coronary syndrome: A network meta-analysis of 61 898 patients from 15 randomized trials. Eur Heart J. 2022;43:959-967. doi: 10.1093/eurheartj/ehab836
- [CrossRef] [PubMed] [Google Scholar]
- Pharmacokinetics and pharmacodynamics of ticagrelor in the treatment of cardiac ischemia. Expert Opin Drug Metab Toxicol. 2016;12:1491-1502. doi: 10.1080/17425255.2016.1244524
- [CrossRef] [PubMed] [Google Scholar]
- Brilique® (ticagrelor) product monograph. 2016. Tablets for oral use 60mg and 90 mg. Available from: https://www.ema.europa.eu/en/documents/product-information/brilique-epar-product-information_en.pdf [Last accessed on 2023 Nov 30]
- [Google Scholar]
- 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2020;42:1289-1367. doi: 10.1093/eurheartj/ehaa575
- [CrossRef] [PubMed] [Google Scholar]
- Heart disease and stroke statistics-2020 update: A report from the American Heart Association. Circulation. 2020;141:e139-e596. doi: 10.1161/CIR.0000000000000757
- [CrossRef] [Google Scholar]
- ICMR Guidelines. 2017. Available from: https://main.icmr.nic.in/sites/default/files/guidelines/ICMR_ethical_guidelines_2017.pdf [Last accessed on 2023 Nov 30]
- [Google Scholar]
- New drugs and clinical trials rules 2019 India. Perspect Clin Res. 2020;11:37-43. doi: 10.4103/picr.PICR_208_19
- [CrossRef] [PubMed] [Google Scholar]
- World Medical Association declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79:373. doi: 10.1001/jama.2013.281053
- [CrossRef] [PubMed] [Google Scholar]
- E6: Guidance on good clinical practice. 2002. PMP/ICH/135/95). Netherlands: European Medicines Agency; Available from: https://www.imim.cat/media/upload/arxius/emea.pdf [Last accessed on 2023 Nov 30]
- [Google Scholar]
- Bioequivalence assessment of two ticagrelor formulations under fasting condition in healthy Pakistani subjects. Pak J Med Sci. 2023;39:1647-1651. doi: 10.12669/pjms.39.6.8203
- [CrossRef] [Google Scholar]
- Bioavailability and bioequivalence studies In: Pharmaceutical formulation design-recent practices. United Kingdom: IntechOpen; 2020. doi: 10.5772/intechopen.85145
- [CrossRef] [Google Scholar]
- Committee for medicinal products for human use (CHMP) EMA/CHMP/177281/2016/Corr. Ticagrelor product-specific bioequivalence guidance. Available from: https://www.europa.eu [Last accessed on 2023 Nov 30]
- [Google Scholar]
- Pharmacokinetics, bioequivalence and safety evaluation of two ticagrelor tablets under fasting and fed conditions in healthy Chinese subjects. Drug Des Devel Ther. 2021;15:1181-1193. doi: 10.2147/DDDT.S297918
- [CrossRef] [Google Scholar]
- Bioequivalence study of two formulations of rivaroxaban in healthy adult subjects under fasting conditions. Am J Pharmacother Pharm Sci. 2023;2:1-8. doi: 10.25259/AJPPS_2023_008
- [CrossRef] [Google Scholar]
- Bioequivalence study of diclofenac 150 mg XR: A single-dose, randomized, open label, 2-period crossover study in healthy adult volunteers. J Biosci Med. 2023;11:23-32. doi: 10.4236/jbm.2023.1111003
- [CrossRef] [Google Scholar]
- Bioequivalence assessment of two formulations of empagliflozin in healthy adult subjects. Am J Pharmacother Pharm Sci. 2023;19:1-7. doi: 10.25259/AJPPS_2023_019
- [CrossRef] [Google Scholar]
- FDA product-specific guidances for generic drug development web page. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/psg/ticagrelor_oral%20tablet_nda%20022433_rv07-18.pdf [Last accessed on 2023 Dec 04]
- [Google Scholar]






