Translate this page into:
Enhancing clinical management of neurological disorders: Feedback from the healthcare provider perspective
*Corresponding author: Mitali Kapoor, Ph.D, Medical Affairs Department, Medisage E-Learning Pvt. Ltd, Mumbai, Maharashtra, India. mitali.kapoor@mymedisage.com
-
Received: ,
Accepted: ,
How to cite this article: Sultana S, Gite MR, Tawde AD, et al. Enhancing clinical management of neurological disorders: Feedback from the healthcare provider perspective. Am J Pharmacother Pharm Sci 2024:7.
Abstract
Objectives:
Neurological disorders are a global health concern, and their management requires competent health-care professionals (HCPs). This study aimed to evaluate the current state of neurological case management among Indian HCPs by focusing on different aspects such as frequency of encounters, confidence, and upskilling preferences in managing neurological cases.
Materials and Methods:
A quantitative cross-sectional survey was conducted among 104 HCPs, including general practitioners (GPs) and consulting physicians (CPs). The survey gathered data on the frequency of encountering neurological cases, confidence levels, areas for improvement, preferred upskilling methods, and willingness to seek guidance from neurology experts.
Results:
Of the 104 HCPs surveyed, 69 (66.35%) HCPs frequently encountered neurological cases in their daily practice. Among them, 70.19% expressed a moderate level of confidence in managing such cases. Nearly, all HCPs (99.04%) showed a keen interest in upskilling their expertise in the field of neurology. The preferred approaches for upskilling included case-based learning (38.38%) and online webinars or lectures (38.38%). In addition, they showed a willingness to engage with neurology experts for guidance.
Conclusion:
Our study results highlight the high prevalence of neurological cases in the daily practices of HCPs. The findings reveal that HCPs are moderately confident in managing these cases, underscoring the necessity for targeted interventions to enhance their proficiency. Overall, the study emphasizes the importance of tailored neurological interventions to address the specific needs of Indian HCPs in managing neurological cases.
Keywords
Neurological disorders
Health-care professionals
Competence
Upskilling
Interdisciplinary collaboration
INTRODUCTION
Neurological disorders are the second largest cause of mortality worldwide.[1] Although the age-standardized incidence, mortality, and prevalence rates of numerous neurological problems decreased in many countries between 1990 and 2015, the absolute number of individuals affected by, dying from, or staying incapacitated from neurological disorders has increased internationally during the last 25 years.[1] Two reports issued by the World Health Organization (WHO) and the World Federation of Neurology, highlight the public health issues encountered when addressing neurological disorders, especially in developing countries with limited resources.[2-4]
Approximately 30 million of India’s population currently suffer from neurological disorders, according to data from house-to-house surveys conducted in 6 studies.[5-10] Since neurological infections, traumatic injuries, neoplasms, and metabolic abnormalities were not covered in the surveys, the burden of neurological disorders is underestimated.[2] The rates of overall prevalence (3.0–11.9/1,000 population) and incidence (0.2–0.6/1,000 population/year) in the general population show similarities to those in high-income countries (HICs), even with noticeable differences in population characteristics.[11] In India, like in other developing nations, there is a scarcity of qualified neurologists, necessitating ground plans and policies tailored to the socioeconomic and cultural context for undertaking neuro-epidemiological investigations.[2]
In terms of individuals seeking medical guidance from a general practitioner (GP), neurological conditions emerge as the third most commonly reported concern. According to a study, due to inadequate training, lack of experience, and misunderstandings about functional neurological disorders, many medical practitioners are hesitant to handle patients with this condition.[12] Even the process of conveying the diagnosis and exploring treatment options can present significant difficulties.[12] Another study showed that psychiatrists had the lowest level of confidence when it came to their abilities to conduct neurological examinations and understand neuroanatomy.[13] In a survey examining attitudes toward functional seizures, more than half of GPs expressed uncertainty or disbelief regarding the involuntary nature of such seizures.[14]
Evidence-based practice is widely recognized as the gold standard when providing effective and safe health care. This requires professionals to update and upskill themselves on current evidence and to change their practice to align with this, as well as with their patient’s preferences.[15]
Given the prevalent misconceptions and uncertainties among health-care professionals (HCPs) regarding neurological conditions, there is a pressing need to improve their knowledge, skills, and confidence in managing these cases effectively. The aim of this study was to evaluate the current state of neurological case management among Indian HCPs by focusing on different aspects such as frequency of encounters, confidence, and upskilling preferences in managing neurological cases.
MATERIALS AND METHODS
Study design and population
The study was conducted in India and targeted HCPs across various regions of the country. An online cross-sectional survey was conducted among 104 HCPs to assess various aspects of neurological cases, including their frequency, proficiency of Indian HCPs in managing them, their engagement in upskilling activities, areas of knowledge enhancement, and concerns in this field. This study utilized a web-based self-report survey approach, incorporating semi-structured quantitative surveys to gather data from a diverse group of HCPs across various regions of India.
Study population
The study population consisted of health professionals, including GPs, consulting physicians (CPs), and neurologists, who participated in this survey from March to June 2023. The inclusion criteria required all participants to be qualified HCPs who delivered neurological care to individuals, and to be actively practicing. There were no other restrictions and participation was voluntary. The participants who did not meet the inclusion criteria were excluded from the study.
Data collection
The web-based survey questionnaire was made available on the homepage of the official website of the MediSage app and remained online for approximately 4 months. Multiple methods were employed to reach out to the HCP groups. These methods include a pop-up on the Medisage App, through which HCPs could voluntarily participate in the survey. Reminder notifications were sent through in-app and WhatsApp to a predetermined list of HCPS from the database. Participants were assured of data confidentiality and required to provide consent before participating in the study.
Reminder notifications were sent every 2 weeks to encourage participation. No incentives were offered in return for completing the questionnaire.
Survey design and development
The questionnaire was designed following an extensive review of prior studies examining clinician responses to neurological cases. Three members of the research team conducted an initial review to ensure content and face validity. The questionnaire underwent revisions based on feedback received to enhance its robustness as a research tool for assessing HCPs’ perspectives on neurological care.[13,16,17]
The survey comprised ten questions addressing participants’ professional designation, frequency of encountering neurological cases, confidence in managing such cases, interest in upskilling neurology knowledge, preferred areas of improvement, and desired upskilling activities. The final part of the questionnaire included an open-ended question about barriers and limitations related to upskilling neurology knowledge and managing neurological cases. The survey was thoughtfully structured to collect relevant and reliable data for the study.
Data analysis
The collected survey responses underwent a meticulous data analysis process, utilizing Microsoft Excel for organization and computation. Once the survey data was collected, it was anonymized and organized into a structured format within the spreadsheet. Descriptive statistical methods were employed to understand the participants’ responses quantitatively. This integrated approach provided a comprehensive understanding of the participants’ perspectives on upskilling in neurology and managing neurological cases.
RESULTS
Participant demographics
A total of 104 HCPs participated in the survey, with the majority being CPs at 61.54%, followed by GPs at 31.73%. A smaller percentage of participants represented diabetologists (1.92%), general surgeons (2.88%), and professors of medicine (1.92%). These participants were drawn from highly reputable hospitals.
Frequency of neurological cases
According to the survey, a substantial majority of HCPs, approximately 66.35%, indicated frequent encounters with neurological cases during their professional experience. In contrast, a smaller proportion, specifically 25% of HCPs, reported occasional encounters of neurological cases. Surprisingly, only a few HCPs (5.77%), reported a high frequency of encountering neurological cases. The data based on specialization revealed that 71.88% of CPs frequently encountered neurological cases, while 48.48% of GPs frequently encountered such cases within their clinical practice (P = 0.0232) [Table 1].
| Specialty | Total neurological cases encountered (%) | Cases encountered by GPs (%) | Cases encountered by CPs (%) | Value of Significance (P<0.05) |
|---|---|---|---|---|
| Very frequently | 6 (5.77) | 6.06 | 6.25 | 0.9681 |
| Frequently | 69 (66.35) | 48.48 | 71.88 | 0.0232 |
| Occasionally | 26 (25.00) | 39.39 | 20.31 | 0.04444 |
| Rarely | 3 (2.88) | 6.06 | 1.56 | 0.22628 |
HCPs: Health-care professionals, CPs: Consulting physicians, GPs: General practitioners
HCP’s confidence in managing neurological cases
When the confidence levels of HCPs in managing neurological cases were assessed, it was found that 70.19% showed a moderate level of confidence in handling such cases, while 23.08% reported a high level of confidence. When examining the responses from two distinct medical specialties, CPs, and GPs, it was observed that 84.85% of GPs and 67.19% of CPs reported having a moderate level of confidence in handling neurological cases (P = 0.062; confidence interval [CI] 95%). Notably, 26.56% of CPs were very confident in managing these cases (P = 0.015; CI 95%). While a non-significant proportion of HCPs (P > 0.05; CI 95%) were not confident in handling the neurological cases.
HCPs Preferences for upskilling in neurology
According to the survey results, 103 (99.04%) HCPs expressed a strong interest in improving their knowledge and skills in the field of neurology [Figure 1a]. A detailed analysis based on specialty revealed that a significant number of CPs (98.44%) showed an interest in upskilling their knowledge in this field. GPs demonstrated a high level of enthusiasm for upskilling in this domain, with the entire cohort of GPs (100%) displaying a keen interest in enhancing their neurological knowledge and competencies.
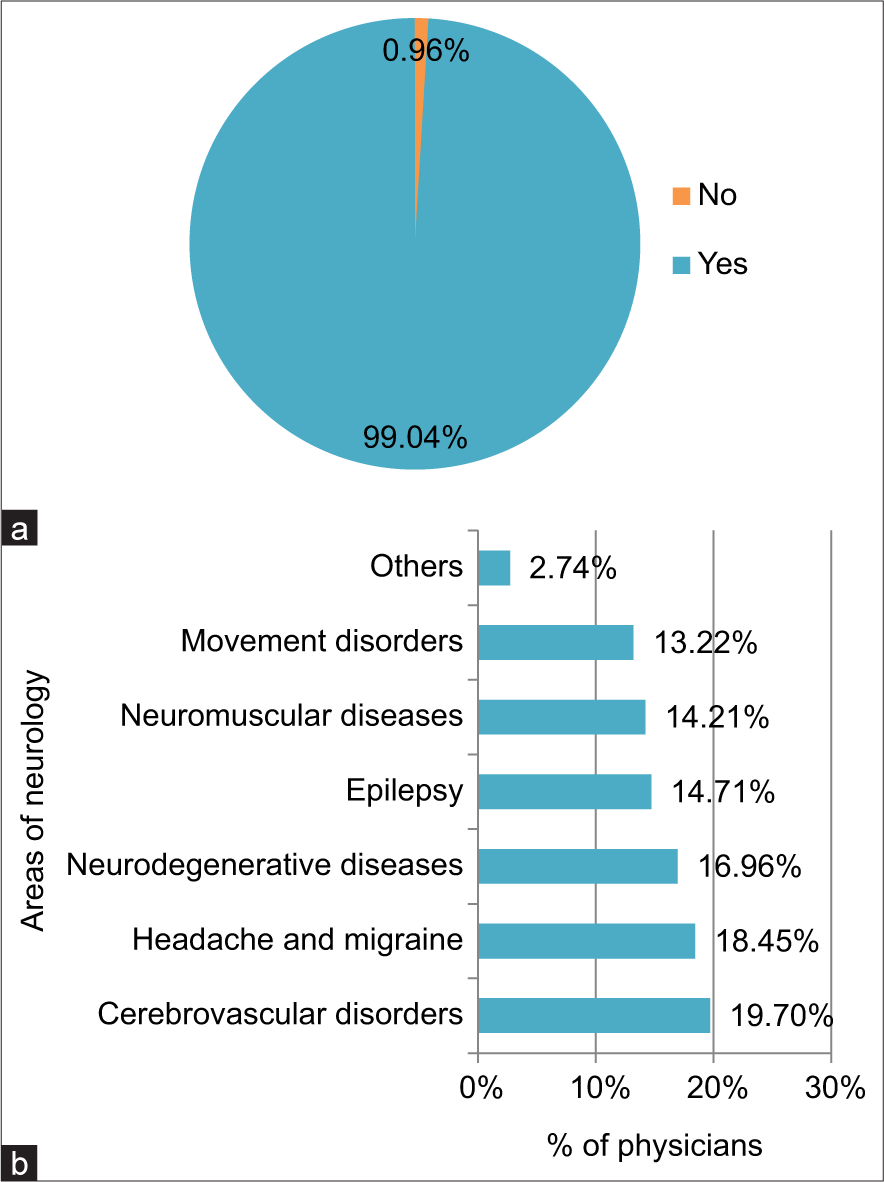
- (a) Health-care professionals (HCP’s) interest in upskilling knowledge in the neurological field (b) distribution of upskilling requirements across different areas of neurology among HCPs.
Our survey results assessing upskilling requirements across various domains of neurology revealed that 19.70% of HCPs sought to enhance their understanding of cerebrovascular disorders, while 18.45% expressed interest in the field of headaches and migraines. In addition, 16.96% desired upskilling in neurodegenerative diseases, 14.71% in epileptic disorders, 14.21% in neuromuscular conditions, and 13.22% in movement disorders [Figure 1b].
On further analysis of knowledge improvement areas by specialties, it was observed that both CPs and GPs had a preference for enhancing their knowledge in neurology areas, including headache and migraine (>20%) and cerebrovascular diseases (>18%). Subsequent areas of interest encompassed neuromuscular diseases, neurodegenerative diseases, movement disorders, and epilepsy for both CPs and GPs [Figure 2]. Furthermore, GPs and CPs expressed interest in enhancing their proficiency in several specific neurology domains. These areas of interest encompassed upper and lower motor neuron diseases, spinal cord disorders, emergency basis intensive care unit cases, neurological spine, peripheral neuropathy, intracranial space-occupying lesions, paralysis, and ophthalmic pain.
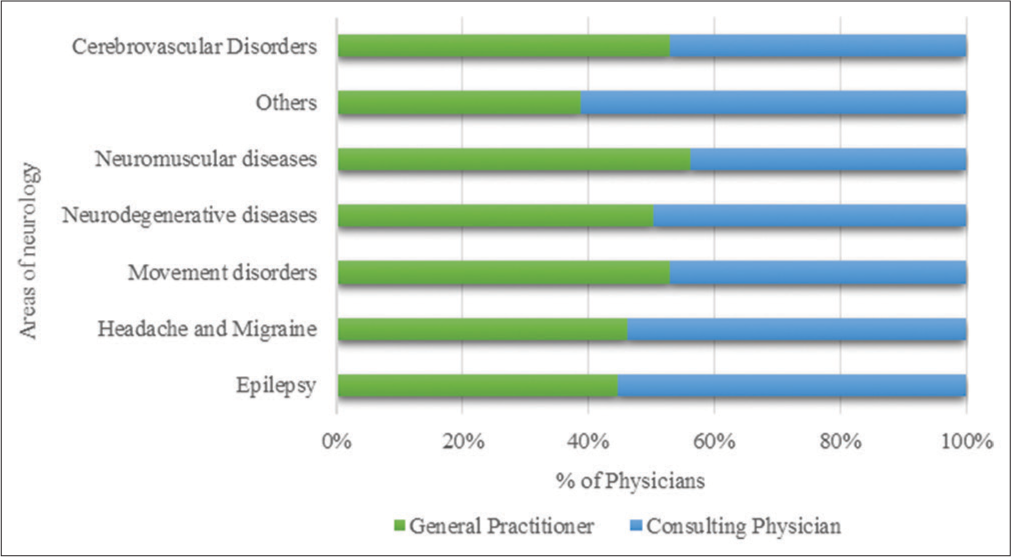
- Distribution of upskilling requirements across different areas of neurology among consulting physicians and general practitioners.
Analyzing the preferred upskilling activities among HCPs is crucial for designing effective professional development programs. The survey findings demonstrated that HCPs had a preference for case-based learning and online webinars or lectures, thus highlighting the importance of interactive and easily accessible learning formats, especially for professionals with busy schedules [Figure 3a]. Furthermore, the survey indicated that in-person discussions with experts and peer-to-peer learning were also highly valued, emphasizing the significance of interpersonal engagement and knowledge sharing in the upskilling process. In addition, when considering specialties, there were variations in the preferred upskilling methods between CPs and GPs. CPs primarily favored online lectures and webinars (34.40%) and case-based learning (39.20%) for their upskilling activities, while the majority of GPs (69%) leaned toward online lectures and webinars as their preferred methods for upskilling [Figure 3b].
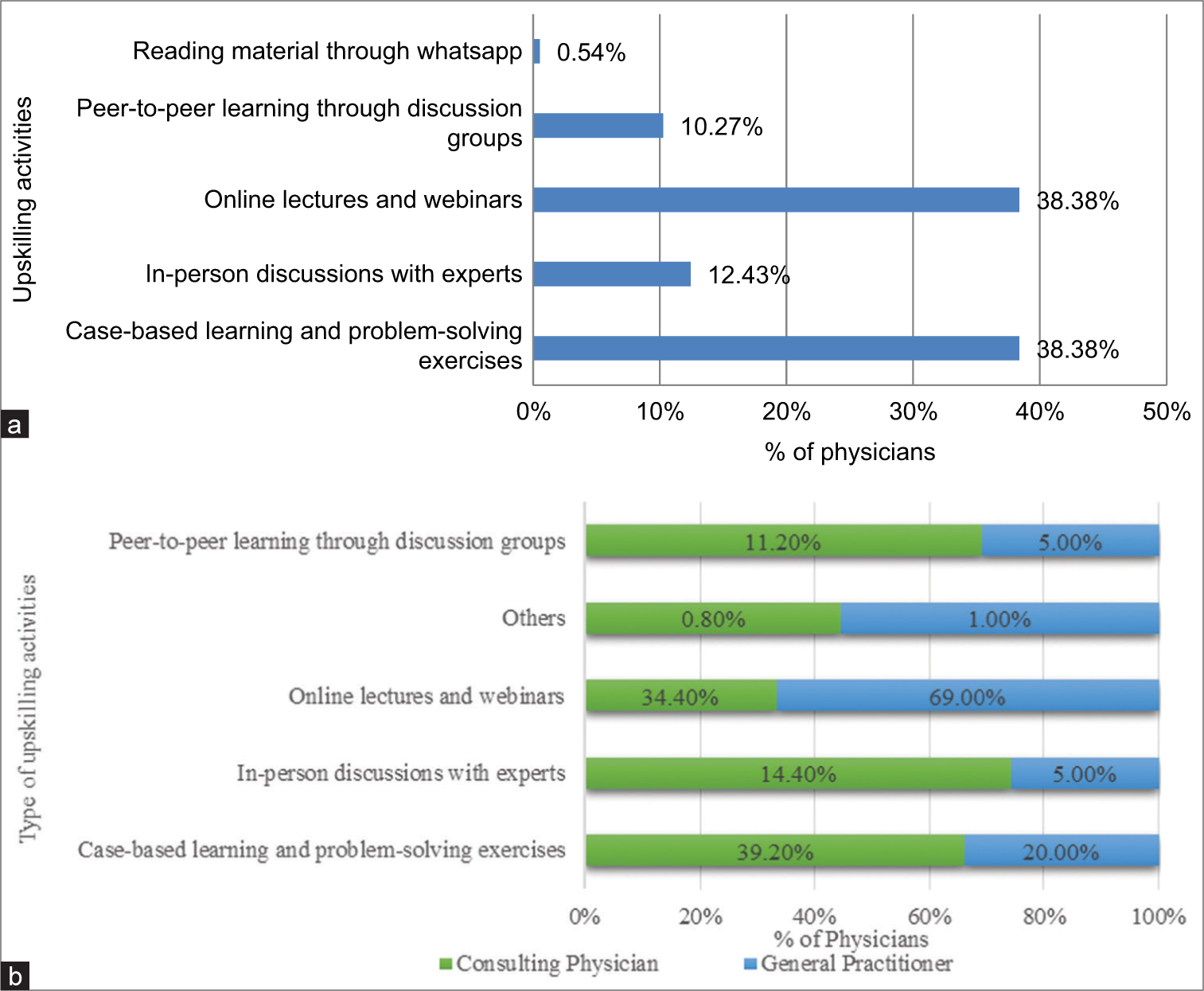
- (a) Learning channels for upskilling activities among health-care professionals. (b) Learning channels for upskilling activities among consulting physicians and general practitioners.
HCPs interest in interdisciplinary communication
The surveyed HCPs demonstrated diverse preferences when seeking guidance on neurological cases. Over 55% favored consulting neurologists, while <25% preferred neuropsychologists. Furthermore, <20% of HCPs chose to consult neurosurgeons for guidance on neurological cases [Figure 4].
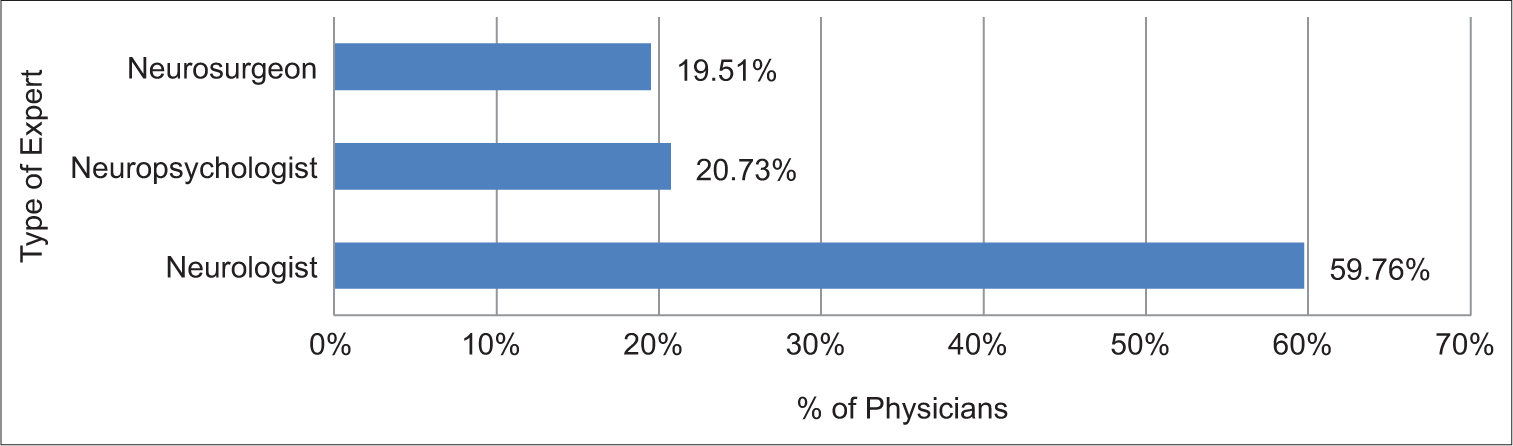
- Preferred neurology expert for discussing questions or concerns.
To understand the importance of fostering communication and collaboration between medical specialties, HCPs were asked about their interest in discussing their questions or concerns with a neurology expert. The results showed that a substantial percentage of HCPs (55.88%) demonstrated a willingness to engage with neurology experts for advice and guidance, indicating a positive inclination toward interdisciplinary communication. However, 30.39% of HCPs expressed uncertainty, and 13.73% explicitly declined such interactions. Based on specialty, a significant proportion of CPs and GPs expressed interest in these discussions (56.25% and 51.52%, respectively), while a substantial number of HCPs, including 31.25% of CPs and 27.27% of GPs, remained uncertain about their participation in such discussions.
DISCUSSION
The findings of our survey help to better understand the capability and preferences of HCPs when it comes to managing neurological cases and their willingness to enhance their expertise in this field. In addition, the interest in seeking expert guidance and the preferred types of neurology experts (Neurologist, Neuropsychologist, and Neurosurgeon) for consultations were also explored.
The study revealed that neurological cases are prevalent among HCPs, including both CPs and GPs, indicating their integral role in daily health-care practices. The study highlights varying levels of confidence among HCPs in managing neurological cases, with the majority expressing a moderate level, but a concerning minority displaying a lack of confidence, raising critical concerns about patient care quality. An overwhelming majority of HCPs exhibit a profound interest in enhancing their knowledge and skills in neurology, with specific domains such as cerebrovascular disorders, headaches, neurodegenerative diseases, epilepsy, neuromuscular conditions, and movement disorders being of particular interest. The study also identifies clear preferences for online lectures, webinars, case-based learning, and problem-solving as preferred methods for upskilling. A significant portion of HCPs had a keen interest in seeking guidance from various neurology experts, including neurologists, neuropsychologists, and neurosurgeons. More than 50% of CPs and GPs are open to engaging in discussions with neurological experts to address their questions and concerns.
The majority of HCPs frequently encountered neurological cases during their professional practice, indicating that they are a common and integral part of the HCPs’ daily practice. Further analysis by specialty found that both CPs and GPs receive neurological cases frequently in their clinical practice. This observation aligns with a study conducted by Morrish, which emphasizes the pivotal role played by GPs in the identification and optimization of care for patients with various neurological conditions. The study suggests that GPs, due to their familiarity with patients’ histories and social contexts, may be better equipped to decide whether to investigate common neurological symptoms.[18]
The study findings revealed varying degrees of confidence among HCPs in their ability to manage neurological cases. While the majority expressed a moderate level of confidence, a significant minority displayed a lack of confidence, raising important concerns regarding the quality of patient care. The results, based on specialty indicate that a significant proportion of GPs possess a moderate level of confidence in handling neurological cases (P = 0.062, CI 95%) than GPs, while only a small fraction of HCPs in each group exhibited higher levels of confidence (P = 0.015, CI 95%). These findings are consistent with prior studies by authors Hutchinson et al., Samanta et al., which demonstrate that primary care providers receive limited exposure to epilepsy management during their neurology clerkships and residencies, consequently resulting in the lower levels of confidence when it comes to handling neurologic conditions.[19,20]
As per the findings derived from the survey, an overwhelming majority of HCPs demonstrated a profound interest in augmenting their knowledge and skill set within the realm of neurology. A large number of HCPs showed interest in upskilling their knowledge across various domains of neurology, including cerebrovascular disorders, headaches and migraines, neurodegenerative diseases, epileptic disorders, neuromuscular conditions, and movement disorders. A cross-sectional survey of 588 practitioners showed a significant gap in adhering to international stroke prevention guidelines. While the majority of practitioners recognize at least one major stroke symptom, only 46% correctly identify all five. Despite regularly monitoring blood pressure, only 63% initiate antihypertensive therapy per guidelines. In addition, 75% neglect routine cholesterol checks, and 36% independently treat stroke patients, emphasizing the need for urgent stroke-related education to bridge the disparity between practice and established guidelines.[21] These findings provide valuable insights that can inform the customization of neurology upskilling initiatives to align with the unique requirements and interests of HCPs. Adapting programs in accordance with these preferences has the potential to enhance the efficacy of training, thereby contributing to the improvement of patient care in these specialized domains of neurology.
HCPs displayed clear preferences when it came to methods for enhancing their skills and knowledge. Our analysis also revealed a substantial inclination among CPs and GPs toward online lectures, webinars, case-based learning, and problem-solving as their preferred modes of upskilling. These findings align with a meta-analysis by McKinney, which showed that HCPs generally find web-based training satisfactory, and this method leads to measurable improvements in their knowledge and behavior.[22] Another study by Ochoa and Wludyka demonstrated that an online interactive educational platform for medical students resulted in a significant enhancement in immediate comprehension of epilepsy when compared to the standard curriculum.[23] The interactive, web-based high-quality teaching has become popular among HCPs due to its flexibility, broad resource-sharing capacity, global reach, and cost-effectiveness.[24] National health-care organizations such as the American Academy of Neurology and American Epilepsy Society have expanded their online offerings, including annual meeting materials, lectures, self-assessment exams, videos, audio files, webinars, and learning modules, to address the educational needs of busy physicians in line with these preferences.[20]
In our survey, 54.16% of HCPs expressed a keen interest in seeking guidance from a range of neurology experts, including neurologists, neuropsychologists, and neurosurgeons. Furthermore, the study’s findings revealed that more than 50% of CPs and GPs were open to engaging in discussions with neurological experts to address their questions and concerns. Recognizing these preferences could serve as a catalyst for promoting effective communication and collaboration among various specialties within the realm of neurology.
Strengths and limitations
This study has several strengths and limitations. On the positive side, the study provides valuable insights into the imperative need for HCP upskilling within the neurology domain. It delves into the specific preferences of HCPs for upskilling across various neurology areas, shedding light on the nuances of their educational requirements. In addition, the study evaluates the capability of CPs and GPs in managing neurological cases, contributing to a comprehensive understanding of their roles in this context. Furthermore, the study uncovers HCPs’ preferred methods for upskilling, which can inform the design of tailored training programs, enhancing their effectiveness in this critical domain.
However, it is essential to acknowledge the limitations of this study. First, the low responses obtained from the survey raise concerns about the representativeness of the findings, as the results may not fully capture the perspectives of all five health-care professions under study. This limitation underscores the need for caution in generalizing the results to HCPs who did not participate.
CONCLUSION
The information obtained from this survey can serve as a foundation for designing targeted educational programs and training initiatives aimed at enhancing the competence of HCPs in neurology. By addressing the identified gaps in knowledge and fostering effective communication channels, HCPs can collaboratively work toward optimizing patient outcomes, improving patient satisfaction, and ultimately advancing the quality of neurological care provided to the community.
Acknowledgment
We express our sincere appreciation to MediSage E-Pvt. Learning for their pivotal role in the execution of this survey manuscript. It is noteworthy that MediSage E-Pvt. Learning has undertaken this survey initiative without any financial gain, demonstrating a commitment to advancing knowledge in the field of neurology. We extend our gratitude to the HCPs who participated in this survey, as their valuable input has been instrumental in shaping the outcomes presented in this manuscript.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’ consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
None.
References
- Global, regional, and national burden of neurological disorders during 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2015;16:877-897. doi: 10.1016/S1474-4422(17)30299-5
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of neurological disorders in India: Review of background, prevalence and incidence of epilepsy, stroke, Parkinson's disease and tremors. Neurol India. 2014;62:588-598. doi: 10.4103/0028-3886.149365
- [CrossRef] [PubMed] [Google Scholar]
- Neurological disorders: Public health challenges. Available from: https://www.who.int/publications/i/item/9789241563369 [Last accessed on 2024 Jan 16]
- [Google Scholar]
- Atlas: Country resources for neurological disorders. 2004. Geneva: World Health Organization; Available from: https://www.who.int/publications-detail-redirect/9241562838 [Last accessed on 2024 Jan 16]
- [Google Scholar]
- Neuroepidemiological study in semi-urban and rural areas in South India: Pattern of neurological disorders including motor neurone disease In: Gourie-Devi M, ed. Motor neurone disease. Global clinical patterns and international research. New Delhi: Oxford and IBH; 1987. p. :11-21.
- [Google Scholar]
- Prevalence of common neurological diseases in rural community of India. Indian J Community Med. 1989;14:171-176.
- [CrossRef] [Google Scholar]
- Prevalence and pattern of major neurological disorders in rural Kashmir (India) in 1986. Neuroepidemiology. 1994;13:113-119. doi: 10.1159/000110368
- [CrossRef] [PubMed] [Google Scholar]
- Neuroepidemiology of major neurological disorders in rural Bengal. Neurol India. 1996;44:47-58.
- [Google Scholar]
- Epidemiological study of neurological disorders in a rural population of Eastern India. J Indian Med Assoc. 2003;101:299-300, 302-304
- [Google Scholar]
- Prevalence of neurological disorders in Bangalore, India: A community-based study with a comparison between urban and rural areas. Neuroepidemiology. 2004;23:261-268. doi: 10.1159/000080090
- [CrossRef] [PubMed] [Google Scholar]
- Epilepsy in India I: Epidemiology and public health. Ann Indian Acad Neurol. 2015;18:263-277. doi: 10.4103/0972-2327.160093
- [CrossRef] [PubMed] [Google Scholar]
- Survey of the perceptions of health practitioners regarding functional neurological disorders in Australia. J Clin Neurosci. 2019;67:114-123. doi: 10.1016/j.jocn.2019.06.008
- [CrossRef] [PubMed] [Google Scholar]
- Unveiling the enigma: Physicians' perceptions of functional neurological disorders in Egypt-a cross-sectional study. Egypt J Neurol Psychiatry Neurosurg. 2023;59:96. doi: 10.1186/s41983-023-00697-5
- [CrossRef] [Google Scholar]
- Functional seizures: An evaluation of the attitudes of general practitioners local to a tertiary neuroscience service in London. Epilepsia Open. 2018;4:54-62. doi: 10.1002/epi4.12283
- [CrossRef] [PubMed] [Google Scholar]
- Upskilling health and care workers with augmented and virtual reality: Protocol for a realist review to develop an evidence-informed programme theory. BMJ Open. 2021;11:e050033. doi: 10.1136/bmjopen-2021-050033
- [CrossRef] [PubMed] [Google Scholar]
- A survey of physicians' perception of the use and effectiveness of diagnostic and therapeutic procedures in chronic cough patients. Lung. 2021;199:507-515. doi: 10.1007/s00408-021-00475-1
- [CrossRef] [PubMed] [Google Scholar]
- Physician perceptions of performance feedback and impact on personal well-being: A qualitative exploration of patient satisfaction feedback in neurology. Jt Comm J Qual Patient Saf. 2023;49:138-148. doi: 10.1016/j.jcjq.2022.12.003
- [CrossRef] [PubMed] [Google Scholar]
- The changing relationship between neurology and general practice in the UK. Br J Gen Pract. 2009;59:599-604. doi: 10.3399/bjgp09X453837
- [CrossRef] [PubMed] [Google Scholar]
- Identification and referral of patients with refractory epilepsy from the primary to the tertiary care interface in New South Wales, Australia. Epilepsy Behav. 2020;111:107232. doi: 10.1016/j.yebeh.2020.107232
- [CrossRef] [PubMed] [Google Scholar]
- Healthcare professionals' knowledge, attitude, and perception of epilepsy surgery: A systematic review. Epilepsy Behav. 2021;122:108199. doi: 10.1016/j.yebeh.2021.108199
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge gaps in stroke care: Results of a survey of family physicians in Pakistan. J Stroke Cerebrovasc Dis. 2011;20:282-286. doi: 10.1016/j.jstrokecerebrovasdis.2010.01.010
- [CrossRef] [PubMed] [Google Scholar]
- Assessing the evidence for the educational efficacy of webinars and related internet-based instruction. Pedagogy Health Promot. 2017;3:47S-51S. doi: 10.1177/2373379917700876
- [CrossRef] [Google Scholar]
- Randomized comparison between traditional and traditional plus interactive Web-based methods for teaching seizure disorders. Teach Learn Med. 2008;20:114-117. doi: 10.1080/10401330801989513
- [CrossRef] [PubMed] [Google Scholar]
- Internet-based learning in the health professions: A meta-analysis. JAMA. 2008;300:1181-1196. doi: 10.1001/jama.300.10.1181
- [CrossRef] [PubMed] [Google Scholar]






